- Information
- AI Chat
Chapter 7 - help for uni
Epidemiology (BMS3023)
Newcastle University
Preview text
Critical Appraisal of Epidemiological Studies and Clinical Trials (4 edn) Mark Elwood doi/10.1093/med/9780199682898.001. Published: 2017 Online ISBN: 9780191763045 Print ISBN: 9780199682898 Search in this book CHAPTER
doi/10.1093/med/9780199682898.003.0007 Pages 131–
Published: February 2017
Abstract
Keywords: Confounding, randomisation, restriction, stratification, matching, multivariate models, Mantel-
Haenszel, eect modification, logistic regression
Subject: Public Health, Epidemiology
Collection: Oxford Medicine Online
7 Confounding
Mark Elwood
This chapter gives the denition of confounding, a central issue in epidemiology and its dependence on two associations, with exposure and with outcome. It explains confounding in trials, cohort and case-control studies, and Simpson’s paradox. It explains the ve methods of controlling confounding: restriction, randomisation, stratication, matching and multivariate methods. For randomised trials, the limits of randomisation, residual confounding, pre-stratication, intention-to-treat, management and explanatory trials, pragmatic trials are explained. It shows the Mantel–Haenszel risk ratio or odds ratio, direct and indirect standardisation, and eect modication. Frequency and individual matching, their value and limitations, over matching, confounding by indication, and calculation of matched odds ratio are shown. It explains multivariate methods, including linear, logistic, Poisson, and Cox’s proportionate hazards models, including the relationship between coecients and odds ratios, dummy variables, conditional methods, and propensity scores. Thus it is easy to prove that the wearing of tall hats and the carrying of umbrellas enlarges the chest, prolongs life, and confers comparative immunity from disease; for the statistics shew that the classes which use these articles are bigger, healthier, and live longer than the class which never dreams of possessing such things. —George Bernard Shaw: Preface to ʻThe Doctorʼs Dilemmaʼ; 1906 Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Definition and concepts
The ideal experiment
Human studies
Definition of confounding
Introduction
Confounding is the most challenging issue in the interpretation of studies. This chapter is in three parts. In Part 1 , we will dene confounding and show what eects it can produce. In Part 2 , we will deal with how confounding can be controlled. In Part 3 , we will consider some further applications of the logic of confounding.
Part 1. The fundamentals of confounding
A central concept of science in general, and particularly biology, is the tightly controlled experiment. In the classic laboratory experiment, the investigator uses laboratory rats that have been bred under controlled conditions for many generations, are housed in identical physical environments, are fed and handled in the same way, and are then randomly allocated into the required groups. Observations are then made in a standardized manner, with the observer being ‘blind’ as to the allocation of the animal. The objective is to achieve a situation where the groups of animals dier in terms of only one factor, the exposure factor being tested. Therefore it is easy to accept that a dierence in the outcome between the groups of animals is due either to that exposure factor or to chance. The standardized and blind assessment procedure protects against bias in the observations of outcome (as discussed in Chapter 6 ), and randomization of animals from a common pool protects against there being other factors that dier between the groups (confounding). In observational studies on humans such tight control is not possible, for scientic or more commonly for ethical or logistic reasons. Human subjects will dier from one another much more than the laboratory animals will, and we cannot only attempt to control a few aspects of their environment and activities. The challenge is to conduct studies of free-living human subjects that will still have a high degree of validity. p. 132 We have seen already that the results of a study, in terms of the dierences between the groups being compared, may be due to any of four mechanisms: bias, confounding, chance, or causation. Confounding is dened as (Figure 7) a distortion of an exposure–outcome association brought about by the association of another factor with both outcome and exposure. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Properties of a confounder
Direction of eect
Figure 7.
An example of confounding; if there is a positive association between smoking and obesity, and a positive association between obesity and breast cancer, the observed association between smoking and breast cancer will overestimate the true association. In this situation, obesity is a confounding factor. Confounding is produced by the two simultaneous and independent properties: obesity is associated with the outcome in this study, and independently it is associated with the exposure. The denition of confounding involves a denition of the study hypothesis, because it may be that smoking and obesity are both causal factors for breast cancer. So if we were studying the relationship between obesity and breast cancer in women, we would have to consider smoking as a potential confounding factor. The eects of a confounding factor can be in either direction. In the situation given earlier, the exposed group (smoking subjects) has a higher prevalence of obesity, and obesity is associated with an increase in risk of breast cancer. The net result of this confounding will be to give an apparent excess risk of breast cancer in the smoking subjects. In another situation, consider the relationship of smoking to breast cancer, and the eect of number of children as a confounding factor (Figure 7). Suppose that subjects who smoke have had more children, and that having had more children gives a decreased risk of breast cancer (there is good evidence for this). In this situation, the ‘exposed’ group who smoke will have had more children, and because of this their risk of breast cancer will be reduced. If the null hypothesis of no association between smoking and breast cancer is true, the study will give a spurious indication of a protective eect. If there is a real increase in the risk of breast cancer with smoking, the study will underestimate this risk, and may not show it at all, if it fails to take into account the counteracting eect of the dierence in numbers of children between the smoking subjects and the non-smokers. This can be called negative confounding. The same eect would occur if the exposed group, smokers, had a lower prevalence of a factor that increases breast cancer risk. p. 134 Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Two associations necessary
Confounding in cohort and intervention studies
Figure 7.
Negative confounding: if having had more children decreases the risk of breast cancer, and smokers have had more children than non-smokers, the measure association between smoking and breast cancer will underestimate the true association. How do we know if the two associations critical to confounding exist? The issue is not whether the associations exist in general, for example, whether it is true in general that women who smoke are more obese than non-smokers. That relationship is likely to vary between women of dierent ages, in dierent countries, and so on. That is not so important. The crucial issue is, does the association exist within the study population, within the data used in the analysis? Thus, if within the data set given by a particular study it is true that smokers are more obese than non-smokers, and that obese subjects have a higher incidence of breast cancer, then obesity will be a confounding factor in the relationship between smoking and breast cancer. The only other proviso is that the obesity–breast cancer and obesity–smoking associations must be independent; that is, obesity must be associated with smoking use even in women without breast cancer, and obesity must be related to breast cancer even in non-smokers. This may seem dicult logic, but should be clearer after some examples are presented. A factor is therefore a confounding factor only when the two associations exist—when the factor is associated with both the exposure and the outcome under assessment. Smokers and non-smokers may dier in terms of many other factors; for example, they may dier in the proportion with hypertension. Do we have to consider hypertension as a confounder in assessing the study? The answer is, only if hypertension is itself related to breast cancer. If we have asked data on hypertension in our study, we can assess this by looking at the unexposed women, the non-smokers, and seeing if there is an association between hypertension and breast cancer. If there is not, there is no need to consider hypertension as a confounder: it is associated with the exposure, but not with the outcome. Similarly, the risk of breast cancer is increased in women who have a family history of breast cancer. This will be a confounding factor only if in the study in question the prevalence of a family history of breast cancer diers between smokers and non-smokers. p. 135 Because an understanding of confounding is so important, we will look at a number of simple examples, using both hypothetical and real data. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Real example
The relationships between these factors, low exercise, obesity, and the outcome of myocardial infarction are shown diagrammatically in Figure 7. Low exercise is a risk factor for myocardial infarction, with a true relative risk of 3. Obesity is also a risk factor for myocardial infarction, with a relative risk of 2, this result being derived from a comparison of subtables B 1 and B 2. However, because low exercise and obesity are positively related to each other, the apparent relative risk of low exercise, based on simply comparing all low-exercise subjects with all high-exercise subjects, is 4.
Figure 7.
Confounding: the associations which exist in Table 7. RR = relative risk. Further, we can add the data in subtables B 1 and B 2 to compare all obese subjects with all non-obese subjects: we obtain the apparent risk ratio of 3 for the crude relationship between obesity and myocardial infarction. Thus in this situation there are two independent risk factors for myocardial infarction, low exercise and obesity, which are positively correlated with each other, and therefore each acts as a confounding factor when the relationship of the other to myocardial infarction is assessed. p. 137 Consider now a real example of rather simple confounding, shown in Table 7. This is derived from a 1986 paper in the British Medical Journal, which amongst other comparisons (a third method, lithotripsy, was also assessed) compared the success rate for two dierent surgical procedures in the treatment of renal calculi [ 1 ]. The upper table shows the results as they were described in the summary of the paper. For each surgical technique, open surgery and percutaneous nephrolithotomy, 350 patients were assessed, and the success rates were 78 per cent with open surgery and 83 per cent with percutaneous nephrolithotomy. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
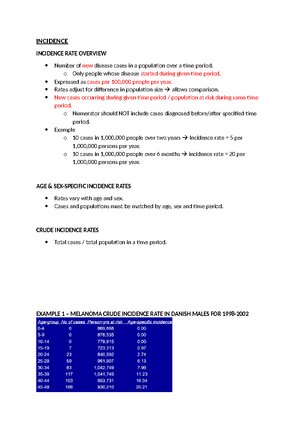
Simpsonʼs paradox
Table 7 Confounding: a comparison of two surgical methods of treating renal calculi, showing success rates (percentage of patients with no stones at 3 months aer treatment). The summary of this paper states ʻsuccess was achieved in 273 (78 per cent) of patients aer open surgery, 289 (83 per cent) aer percutaneous nephrolithotomy.. .ʼ. However, in fact the success rates for open surgery are higher, not lower, than those for the percutaneous technique. The main result of this paper concerns a third method, extracorporeal shock-wave lithotripsy, which was followed by higher success rates than those shown [ 1 ]. Successes Failures Total patients Successes (%) All stones (n = 700) Open surgery 273 77 350 78 Percutaneous nephrolithotomy 289 61 350 83 Stones < 2 cm (n = 357) Open surgery 81 6 87 93 Percutaneous nephrolithotomy 234 36 270 87 Stones ≥ 2 cm (n = 343) Open surgery 192 71 263 73 Percutaneous nephrolithotomy 55 25 80 69 Source: data from Charig CR et al., ʻComparison of treatment of renal calculi by open surgery, percutaneous nephrolithotomy, and extracorporeal shockwave lithotripsy,ʼ The British Medical Journal, Volume 292, Issue 6524, pp. 879–882, © 1989 10.1136/bmj.292.6524 [ 1 ]. In this study, patients were categorized into those who had stones of less than 2 cm in diameter, and those with larger stones. For patients with small stones, the success rate of open surgery was better than that of the other technique, 93 per cent compared to 87 per cent. For patients with larger stones, open surgery also had the higher success rate, 73 per cent compared to 69 per cent. Thus, for either of the two groups of patients, open surgery gave better success rates. An erroneous impression of a lower success rate is created from the pooled data, because open surgery was used much more often on patients with large stones, and those patients had a lower success rate irrespective of the technique used. (As an aside, when this error was pointed out and a more sophisticated analysis suggested, the authors rejected this as ‘... it would only confound the clinicians’ [ 2 ]. In fact, no complex analysis is needed, just a cross tabulation as in Table 7). p. 138 In this situation, the confounding factor produced a reversal in the direction of a relationship: while percutaneous nephrolithotomy had in fact the higher success rate, the uncontrolled confounding by size of stone gave results showing a higher success rate with open surgery. While there is nothing fundamentally dierent in this than in other confounding eects, such a reversal of eect is sometimes called Simpson’s paradox, named from the English statistician Edward Simpson who described confounding in a hypothetical clinical example in a 1951 paper [ 3 ]. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Table 7 Confounding: data from a cohort study of mortality from coronary heart disease and exercise. Confounding by age distorts the association between physical activity and mortality from heart disease. In table A, a comparison of men with light or moderate physical activity with those with heavy activity gives a relative risk of 3. Table B shows that (1) mortality rises with age and (2) the proportion of men doing light or moderate work rises with age. Age is a confounding factor, and its eect gives an increase in the observed relative risk between light activity and CHD mortality. This excess is shown as the relative risks within each of four age bands are all much lower than the crude estimate of 3 [ 4 ]. See also Chapter 4. (page 50–51). Activity level Deaths Man-years Rate/10 000 Relative risk (A) All ages Light or moderate 532 65 000 81 3. Heavy 66 27 700 23 1 (referent) (B) Age bands Age 35– Light or moderate 3 5900 5 1. Heavy 4 8300 4. Age 45– Light or moderate 62 17 600 35 1. Heavy 20 11 000 18. Age 55– Light or moderate 183 23 700 77 1. Heavy 34 7400 45. Age 65– Light or moderate 284 17 800 159 2. Heavy 8 1000 80. Source: data from Paenbarger RS and Hale WE, ʻWork activity and coronary heart mortality,ʼ New England Journal of Medicine, Volume 292, Number 11, pp. 545–550, © 1975 Massachusetts Medical Society 10/NEJM197503132921101. All rights reserved [ 4 ]. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Confounding in case–control studies
Figure 7.
Visual representation of confounding data in Table 7. Source: data from Paenbarger RS and Hale WE, ʻWork activity and coronary heart mortality,ʼ New England Journal of Medicine, Volume 292, Number 11, pp. 545–550, © 1975 Massachusetts Medical Society 10/NEJM197503132921101. All rights reserved [ 4 ]. The logic of confounding in case–control studies is identical to that in cohort studies, but the arithmetic is slightly dierent. Table 7 shows a hypothetical example of a case–control study comparing patients with skin cancer with controls, the exposure of interest being eye colour, in two categories, blue and brown. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
the association between hair colour and skin cancer; showing that eye colour is not a confounder in the relationship between hair colour and skin cancer. The reason eye colour is not a confounder is that although it is associated with hair colour, it is not itself a risk factor for skin cancer, as shown by its true odds ratio with skin cancer being 1. The associations are shown diagrammatically in Figure 7. In fact, the calculation of odds ratio for hair colour within the categories of eye colour was unnecessary. Given that there is no association between eye colour and skin cancer once hair colour was controlled, we can deduce that eye colour cannot be a confounder because it does not t the denition of a confounder: it is not associated with the outcome under study. Therefore the crude odds ratio relating hair colour to skin cancer will not be aected by controlling for eye colour. A further example of confounding in a case–control study, based on real data, will be shown in the ‘Eect modication’ section.
Figure 7.
Confounding: a diagram showing the relationships present in the data given in Table 7.
Part 2. Methods for the control of confounding
Having understood what confounding is, we can consider the methods available to deal with it. There are only ve methods available, as shown in Table 7. In the design of a study we can restrict the participation in the study to certain individuals; we can decide to match individuals in the comparison group to individuals in the group of interest; and we may have the option of doing a randomized intervention study. Irrespective of what has been done at the design stage, when we come to the analysis we may again use restriction to certain individuals in the data set; we may divide the data into subgroups by categories of the confounding factor, which is the process known as stratication; or we may use multivariate mathematical methods to take into account the eect of more than one confounding factor simultaneously. In practice, a combination of these methods is usually used. We will discuss each of these ve methods. p. 142 Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Control of confounding: restriction
Table 7 The methods of controlling confounding: one or more may be used. In the design of the study Restriction Matching Randomization In the analysis of the study Restriction Stratification Multivariate methods Let us go back to our example of a study of smoking and breast cancer, and consider how we could avoid being misled by the eect of obesity or of number of children. One way would be to include in the study only women who were not obese and had not had children. We could do this with either a cohort or a case– control design, and we refer to this method as ‘restriction’. It is clearly an eective method, as it removes the confounding, but obviously the disadvantage is that the study then assesses only the association between smoking and breast cancer in women who are not obese and have not had children. We cannot generalize the study results beyond that population. Suppose instead we do the entire study on women who are obese and have had children. Can there still be confounding? The answer is that there is still potential for confounding. The fact that all the women in the study are obese does not mean they all have the same degree of obesity, and if obesity has a dose–response relationship with breast cancer, and if the degree of obesity is dierent in smokers and non-smokers, there is still potential for confounding. The same applies to the number of children each woman has had. If, however, we restrict the entire study to women who have a body mass index of between 30 and 40 kg/m , and have one or two children, the extra specication in the design will reduce the extent of any confounding. However, such precise restriction would be cumbersome to apply in a practical study. 2 All studies involve some restriction, if only for practical reasons. The source and eligible populations will be restricted in terms of calendar time, geographical location, and frequently other factors such as age. Restriction should also be considered if there may be small groups of individuals whose results may be appreciably dierent from those of the main study population; if the study is unlikely to provide much useful information on these subjects, they may be better excluded. For example, a racial or ethnic group which contributes only a small proportion of subjects may have substantially dierent outcome rates and exposure histories, but there is little value in including such subjects if their total number is likely to be too small for independent consideration. If information on this group is important, a new study design or a modication to include more of these subjects may be needed. p. 143 Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Probabilistic process
The value of randomization
Example: iron cooking pots
p. 144 The essential logic is that random allocation makes it likely that the two groups created will be similar in respect of any particular variable. The essential limitation of randomization is that it is a method based on probability. Therefore its chances of success will be great only if substantial numbers of subjects are used, and we can never be certain that randomization will provide equivalent groups. In the extreme, randomization in a study of only two individuals may protect against investigator bias in the assignment, but does not reduce the dierences between the two subjects. In a large randomized study, it is highly likely that the groups created by randomization will be comparable with respect to specic factors. If, however, the numbers in each group are relatively small, (a reasonable guideline might be numbers less than 100), then it is quite likely that purely by chance the groups will still vary. If they vary in terms of a factor which is strongly related to the outcome in the study, that factor will be a confounding factor, and we must deal with that in the analysis. The practical message is that randomization is a valuable technique, which with reasonable numbers of subjects should work in most situations; but we should not assume that simply because randomization has been used, the groups being compared cannot dier in terms of any confounding factor [ 6 ]. Just as in any other study, data on the factors likely to be the main confounders should be used to compare the groups to make sure they are similar. If they are not, even in a randomized study, other methods of analysis such as stratication or multivariate methods may also be used to take account of any dierences of confounding factors. Table 7 shows the value of randomization. In a study previously mentioned in Chapter 3 , the provision of iron rather than aluminium cooking pots to families was assessed as a method of reducing anaemia and improving growth in children in Ethiopia [ 7 ]. A randomized controlled trial was used, the randomization being by household, with one child per household participating. Without randomization, the families using iron pots and those using aluminium pots could dier in terms of a wide range of characteristics, which could be themselves related to child development. Table 7 shows that the groups created by the randomization process are very similar in terms of the age, sex, height, and weight of the children, their recent medical history, characteristics of the mother, and of household access to clean water and sanitation. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Table 7 The benefits of randomization: in a trial in Ethiopia assessing whether the use of iron pots or aluminium pots aected anaemia and weight gain in children, households were randomly allocated to receive either iron or aluminium pots, and one child per household participated in the study. These data show the similarity of the two groups in regard to characteristics at the time of randomization. SD = standard deviation [ 7 ]. Randomized to iron pots (n = 195) Randomized to aluminium pots (n = 212) Age (months, mean and SD) 31 (14) 30 (15) Male/female (numbers) 99/96 106/ Weight (kg, mean and SD) 11 (2) 11 (2) Length (cm, mean and SD) 87 (8) 88 (8) III in week preceding study 57 (29%) 70 (33%) Diarrhoea in week preceding study 35 (18%) 40 (19%) Mother literate 72 (37%) 68 (32%) Mother ill in last 7 days 50 (26%) 49 (23%) Access to clean water 148 (76%) 157 (74%) Adequate sanitation 57 (29%) 72 (34%) Source: data from Adish AA et al., ʻEect of consumption of food cooked in iron pots on iron status and growth of young children: a randomised trial,ʼ The Lancet, Volume 353, Issue 9154, pp. 712–716, © 1999 10/S0140-6736(98)04450-X [ 7 ]. We can look at these two groups of subjects and consider whether, if they were subsequently treated in an identical manner, we should expect their outcomes to be the same; there is little in the table that would suggest otherwise. Randomization is the simplest way to achieve such equivalent groups. In principle, we could have a design where the rst family seen was allocated an iron pot, and was matched to another family on the features shown in Table 7 which would be given an aluminium pot, but such a study would be dicult or impossible to do. The results of this study were that children in households using iron pots had a greater rise in haemoglobin concentration and gained more in both weight and height over a 12- month period, so it was concluded that the provision of iron cooking pots may be a useful way to prevent iron deciency anaemia in similar less developed countries [ 7 ]. p. 145 There is one advantage of randomization that is shared by no other technique. This is that randomization, given reasonably large numbers of subjects, is likely to produce groups that are similar even in respect of variables that we have not anticipated, dened, or measured. Suppose that after the study just described is completed, evidence appears that an infection common in this community is a strong predictor of childhood anaemia. The study would have been better if that infection had been assessed, and if it were shown that the groups were similar in terms of it. But even without those data, as the original study was randomized and had adequate numbers, we can be reasonably sure that the distribution of the two groups in terms of this unmeasured factor would have been similar. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Remaining dierences
Example: diabetes trial
p. 147 Randomization achieves its objectives by a random process. The principle is that it is likely that the groups produced by randomization will be equivalent. But some dierences between the groups will remain, and on some occasions these dierences may be substantial and important. Table 7 shows a table of baseline characteristics for subjects in a historically important randomized study of the treatment of diabetes, comparing those randomized to receive diet and tolbutamide (an oral glucose- lowering agent) with those randomized to receive diet plus a placebo; the outcome of interest was subsequent deaths, of which many were from cardiovascular disease [ 11 ]. Comparing these two groups shows that the patients randomized to receive tolbutamide were older, more frequently had a history of digitalis use or angina, and higher proportions had an electrocardiograph abnormality, high cholesterol levels, high glucose levels, increased relative body weight, and arterial calcication assessed by an X-ray of the lower limb. On the other hand, there was a lower proportion with a history of hypertension. With these data, we cannot be condent that if the two treatments used had identical eects, the two groups would show the same results in terms of subsequent mortality. Several of these factors could have considerable eects on subsequent mortality, and the dierences between the groups appear substantial. Table 7 The limits of randomization: this study compared four regimens for the management of diabetes; here the subjects randomized to diet + tolbutamide (an oral glucose-lowering agent) are compared with those randomized to diet + placebo [ 11 ]. Randomized to diet + tolbutamide n = 204 (% of subjects) Randomized to diet + placebo n = 205 (% of subjects) Age > 55 48 41. Digitalis use 7 4. Angina 7 5. ECG abnormality 4 3. Cholesterol > 300 mg/ ml
15 8.
Fasting glucose > 110 mg/100 ml
72 63.
Relative body weight > 1.
58 52.
Arterial calcification 19 14. Hypertension 30 36. Source: data from University Group Diabetes Program, ʻA study of the eects of hypoglycemic agents on vascular complications in patients with adult-onset diabetes II: Mortality results,ʼ Diabetes, Volume 19, Supplement 2, pp. 785–830, © 1970 [ 11 ]. Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
ʻFailureʼ of randomization
Pre-stratification
Analysis of randomized trials: intention-to-treat analysis
p. 148 Sometimes this is loosely referred to as a ‘failure of randomization’, but that is an inappropriate term. The randomization process has been carried out correctly, but being a probabilistic technique it does not guarantee that the groups will be similar in terms of all factors. Statistical tests show that all but one (cholesterol levels) of these dierences are not statistically signicant at the conventional 5 per cent level, in other words, dierences of this or greater magnitude would be expected to occur on more than 5 per cent of occasions. However, that is not the relevant issue; the relevant issue is whether the dierences are suciently large to inuence the subsequent outcome rates in the two groups: a small dierence in a factor which is strongly related to outcome will be important. Thus in Table 7 we have a randomized study in which there are important dierences between the groups being compared. The results of this study showed that total deaths, and particularly deaths from cardiovascular disease, were substantially higher in the group treated with tolbutamide than in the placebo group. The crucial question is whether this dierence in mortality can be attributed to the tolbutamide, or whether it is due to the other factors that dier between the two groups. As will be shown later in this chapter, other analytical techniques can be used to address this question. It follows from this that where some major confounding factors can be predicted in advance, it may be better not to rely only on the randomization procedure to produce similar groups [ 6 ]. A more reliable procedure is to group the eligible subjects within categories of the strong confounder, and randomize within these categories. Thus in the earlier example we could classify all study entrants by stage of disease, and randomize within each stage, thus ensuring that the stage distribution of the treatment groups will be virtually identical. This is a combination of randomization and stratication, and is sometimes referred to as randomization within blocks, or pre-stratication. For example, in a trial of perineal pain relief after childbirth, women were randomized within four strata, determined by parity (rst birth and later births) and mode of birth (spontaneous and instrumental), as these factors were important in regard to perineal trauma and pain [ 12 ]. However, randomized trials are often dicult and time-consuming in practice, and in clinical studies simple designs have great advantages, and pre-stratication should be used cautiously. It is often used to randomize within centres in multicentre studies, ensuring that each centre treats similar numbers of subjects on each of the alternative therapies. Not all individuals will complete the treatment to which they have been randomized. Some patients may start the treatment but not complete it; they may decide to discontinue, either for reasons related to the treatment (e. side eects) or for other reasons (e. change of residence), or their clinical situation may change so that a change in treatment is indicated. Some patients may be randomized but not even commence treatment. Consider Figure 7. This represents a clinical trial in which patients are randomized into two treatment groups, but only some of the patients complete the course of treatment oered. The question is: to assess the eect of the new therapy, which groups of patients should be compared? p. 149 Downloaded from academic.oup/book/24610/chapter/187902441 by University of Newcastle user on 06 January 2024
Chapter 7 - help for uni
Module: Epidemiology (BMS3023)
University: Newcastle University

- Discover more from: