- Information
- AI Chat
Was this document helpful?
Final pharm exam review
Course: Pharmacology II (NUR 354)
409 Documents
Students shared 409 documents in this course
University: Arizona College of Nursing
Was this document helpful?

PHARM EXAM 3 REVIEW
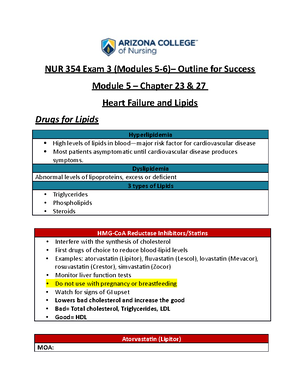
Statins –
• Example ->Atorvastatin
• Used for hyperlipidemia
• Labs to check -> lipid panel
• What will make the doctor order it? LDL HDL triglycerides labs!!
• Once on statin, monitor labs every 3 to 6 months -> need to be educated to get labs
checked frequently
• Once on them they are on them for life
• SE: rhabdo-> sign of muscle breakdown headache, fatigue
• Signs of rhabdo are dark urine and muscle cramping
• Any time a patient starts an anti-lipidemic medication, they need to report any major
side effects such as rhabdo
• Cannot be on it if pregnant
• Educate about diet such as foods that are high cholesterol
• If a patient is old and confused and has dementia you cannot educate them therefore
need to assess their ability to be educated, if they cannot need caregiver to remind
them of things
• Can also be used to prevent MI and strokes
• Antilipidemic
• Hard on the liver should check liver labs
Bile acid sequestrants –
• Cholestyramine: used to excrete cholesterol through stool
• Main side effect is GI upset
• Administered PO -> mix powder with water, two hours before or 4 hours after meals
• If patient is on this medication in terms of coordinating care, who will you go to? ->
dietician
Loop –
• Bumetanide (Bumex):
• Furosemide (Lasix): know Lasix is working if there is urine output
• Monitor urine output usually hourly, 30 ML per hour
• Do daily weights on these patients
Ace Inhibitors (ACEI)–
• Lisinopril: used for hypertension or heart failure
• SE: angioedema and dry cough