- Information
- AI Chat
430 Exam 1 Study Guide
Adult Health Nursing II (NSG-430)
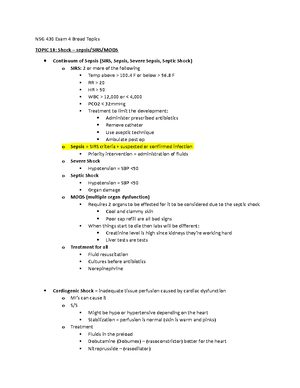
Grand Canyon University
Preview text
Disease: Diabetic Ketoacidosis (DKA)
Pathophysiology Signs and Symptoms Diagnostic Tests
Profound deficiency of insulin characterized by: - Hyperglycemia (≥250) - Ketosis (⬆ ketones) - Acidosis (<7 pH, <16 bicarb) - Dehydration
Sudden onset
Dehydration
Lethargy
Flushed/Dry skin
Sunken eyes
Abd pain, anorexia, N/V
Kussmaul respirations
Acetone/Sweet fruity breath
Rapid, weak pulse
Thirst (polydipsia)
Frequent urination (polyuria)
History and physical examination
Blood studies, including blood glucose, CBC, pH, ketones, electrolytes, BUN, arterial or venous blood gasses
Urinalysis, including specific gravity, glucose, acetone
Risk Factors Complications RN Interventions + Patient Teaching
- Type 1 diabetic
- Illness, infection, or stress
- Inadequate insulin dosage
- Undiagnosed type 1 diabetes
- Poor self management
- Neglect
Hospitalize the client for severe fluid and electrolyte imbalances, fever, N/V, diarrhea, altered mental status. - Unstable treated in ICU
Hypokalemia
Rapid drops in blood glucose causing cerebral edema
A blood glucose reduction of 36 to 54 mg/dL per hour will avoid complications.
Ensure airway (nasal cannula or non-rebreather mask)
Establish IV access, begin fluids
Identify history of diabetes, time of last food, and time and amount of last insulin injection.
Monitor vital signs, level of consciousness, ECG, O2 saturation, and urine output.
Assess breath sounds for fluid overload.
K+ replacement as needed. Always measure K+ levels before starting insulin. Insulin further depletes K+ causing life-threatening hypokalemia.
Medication and Treatments
- Begin fluid resuscitation with 0% NaCl solution (isotonic) 1 L/hr until BP stabilizes and urine output 30-60 mL/hr.
- Begin continuous regular insulin drip 0 U/kg/hr.
- Give potassium to correct hypokalemia.
- Give sodium bicarbonate if severe acidosis (pH <7).
- Add dextrose to IV fluid for blood glucose <250 mg/dL.
Disease: Hyperosmolar Hyperglycemia Syndrome (HHS)
Pathophysiology Signs and Symptoms Diagnostic Tests
A life-threatening syndrome that occurs with diabetes (usually type 2) in a patient that can produce just enough insulin to prevent DKA, but not enough to prevent severe hyperglycemia, osmotic diuresis, and extracellular fluid loss.
- Gradual onset
- Severe dehydration
- BG >
*Ketones are not present, and hypokalemia is not as significant in HHS
- History and physical examination
- Blood studies, including blood glucose, CBC, pH, ketones, electrolytes, BUN, arterial or venous blood gasses
- Urinalysis, including specific gravity, glucose, acetone
Risk Factors Complications RN Interventions + Patient Teaching
>60 years old
Type 2 diabetes
UTI, pneumonia, sepsis, acute illness
Newly diagnosed type 2 diabetes
Impaired thirst response/function
Fewer signs and symptoms lead to BG >600 mg/dL
This can lead to neurologic manifestation such as somnolence, coma, seizure, hemiparesis, and aphasia
S/S might look like a stroke!
Monitor electrolytes, BG, and insulin
Assess vital signs, Is&Os, skin turgor, labs, and cardiac monitoring to check the efficacy of fluid and electrolyte replacement.
Frequent assessment of cardiac, renal, and mental status.
Once the patient is stabilized, attempts to detect and correct the underlying precipitating cause should be initiated.
Medication and Treatments
- The management of DKA and that of HHS are similar and include immediate IV administration insulin and either 0% or 0% NaCl.
- HHS usually necessitates greater volumes of fluid replacement. This should be accomplished slowly and carefully.
- Patients with HHS are commonly older and may have cardiac or renal compromise, necessitating hemodynamic monitoring to avoid fluid overload during fluid replacement.
- When blood glucose levels fall to approximately 250 mg/dL (13 mmol/L), IV fluids containing dextrose are administered to prevent hypoglycemia.
Disease: Diabetes Insipidus (DI)
Pathophysiology Signs and Symptoms Diagnostic Tests
A deficiency of the production or secretion of ADH
Thirst (polydipsia)
Polyuria (2-20 L/day)
Low specific gravity <1.
Urine osmolarity of <
Serum osmolality is elevated
Hypernatremia >
Water Deprivation Test and administration of DDAVP (p)
ADH level after analog of ADH (desmopressin)
Risk Factors Complications RN Interventions + Patient Teaching
Tumor, head injury, CNS infection
Renal insensitivity (lithium, renal damage, renal disease)
Dehydration
Hypernatremia
Maintain adequate hydration (IV and PO)
Maintain electrolyte balance
Monitor BP, HR, LOC, and I&O
Monitor specific urine gravity and serum
Medication and Treatments
- DDAVP ➡ hormone replacement ¬ monitor pulse
- Aqueous vasopressin ¬ hormone replacement
- Chlorpropamide and carbamazepine (Tegretol) ¬ decrease thirst associated with central DI.
- Low-sodium diet (no more than 3 g/day) ¬ helps decrease urine output.
- Thiazide diuretics (hydrochlorothiazide, chlorothiazide), reduce flow to the ADH-sensitive distal nephrons.
- If a low-sodium diet and thiazide drugs are not effective, indomethacin (Indocin) may be prescribed.
- Indomethacin (NSAID) ¬helps increase renal responsiveness to ADH.
Disease: Cushing’s Syndrome
Pathophysiology Signs and Symptoms Diagnostic Tests
Cushing Syndrome: Chronic exposure to excess corticosteroids - Most commonly glucocorticoids - Can also be... - Adrenal androgen excess - Mineralocorticoid excess
Cushing Disease: Pituitary tumor
Truncal obesity/weight gain
Thin extremities
Rounding of face (moon face)
Fat deposits on back of neck and shoulders (buffalo hump)
Reddened skin
Purple striae (loss of collagen)
Easy bruising, poor wound healing
Hyperpigmentation
Hyperglycemia
Muscle wasting
Osteoporosis
Polyuria
Malaise
Insomnia
Headache
Anxiety/Poor concentration
Amenorrhea
Decreased libido
Emotional lability
Psychosis Adrenal androgen excess:
- Hirsutism/gynecomastia Mineralocorticoid excess:
- Acne, hypokalemia, HTN
Plasma ACTH levels
- High-normal with Cushing disease (pituitary etiology)
- Low-undetectable with cushing syndrome
Hypokalemia and alkalosis
- Due to ACTH syndrome and adrenal carcinoma
Health hx
Medication use
Risk Factors Complications RN Interventions + Patient Teaching
- Use of prednisone
- Adrenocorticotropic hormone (ACTH)–secreting pituitary adenoma
- Less common: adrenal tumors, ectopic ACTH production by tumors (lung or pancreas) outside the hypothalamic-pituitary-adrenal axis
- Women 20-40 years old
Caution-Rapid Tapering of corticosteroid post op! Monitor for acute adrenal insufficiency - Vomiting, increased weakness - Dehydration, hypotension - Painful joints - Pruritus - Peeling skin - Severe emotional disturbances
Acute care:
- Vital signs
- Daily weights
- Glucose checks
- Assess for inflammation/infection
- Assess for thromboembolism (PE)
- Emotional support
Preoperative care:
- Control HTN and hyperglycemia
- Correct hypokalemia
- High protein diet Postoperative care:
- Increased risk for hemorrhage
- Large rush of hormones into the circulation (24-48 hrs), causing unstable BP, fluid balance and electrolytes
- High dose corticosteroids are given during and after surgery for several days
- Monitor Is & Os
- Obtain urine sample at the same time each morning for cortisol level evaluation and to monitor effectiveness of surgery
- Bed rest until BP is stable
- Monitor for infection
Medication and Treatments
Primary goal of treatment is to normalize hormone secretion. Treatment will depend on the underlying cause: - Pituitary adenoma: removal of tumor via transsphenoidal approach - Radiation is an option for patients who cannot undergo surgery - Open surgical adrenalectomy for adrenal cancer
- Ectopic ACTH-secreting tumors: removal of tumor (when it is still benign)
- Prolonged corticosteroid use: Gradually discontinue medication by reducing dose, then alternate day regimen
- Patients should wear a medical bracelet, avoid extreme temperatures, infection and stress.
- Teach how to adjust medications and when to call the HCP
- Discuss lifetime hormone therapy replacement.
Disease: Hyperthyroidism/Graves’s Disease/Thyrotoxicosis
Pathophysiology Signs and Symptoms Diagnostic Tests
Clinical syndrome of hypermetabolism - Increased T3, T4 or both - Hyperthyroidism and thyrotoxicosis usually occur together Subclinical hyperthyroid: - TSH below 0. - Normal T3 and T Overt hyperthyroid: - Low or undetectable TSH - Elevated T3 and T Graves Disease: Autoimmune disease, develops antibodies to the TSH receptor, stimulating T3 and T4 or both to be released.
Goiter (may have bruit)
Increased metabolism
Sensitive to stimulation
Exophthalmos, lid lag, eyelid retraction
Increased RR/dyspnea with exertion
HTN, rapid pulse, palpitations
Angina, Cardiac hypertrophy
Increased appetite/thirst
Weight loss, Diarrhea
Splenomegaly
Hepatomegaly
Warm moist skin, intolerance to heat
Thin, brittle nails, clubbing
Hair loss, fine, silky hair
Diaphoresis
Pretibial myxedema
Fatigue, weakness, proximal muscle wasting, dependent edema, osteoporosis
Nervous, fine tremor
Personality changes, irritability
Hyperreflexia
Stupor, coma
Menstrual irregularities, amenorrhea, decreased libido, impotence, gynecomastia, decreased fertility
TSH levels (low, <0)
Free thyroxine (free T4) (elevated)
Total T3 and T
Radioactive Iodine uptake (RAIU) — differentiates Grave’s from other types of thyroiditis. The patient with Graves’ disease will show a diffuse, homogeneous uptake of 35% to 95%, whereas the patient with thyroiditis will show an uptake of less than 2%. The person with a nodular goiter will have an uptake in the high normal range.
Risk Factors Complications RN Interventions + Patient Teaching
- Women are 5x more likely to develop Grave’s
- Grave’s = 75% of all hyperthyroid cases
- Iodine insufficiency
- Cigarette smoking
- Infection
- Stressful life events
- Genetic factors
- Other autoimmune diseases (RA, pernicious anemia, SLE, Addison’s, celiac disease, vitiligo)
Acute Thyrotoxicosis or Thyroid Storm
Excessive release of hormones
Life-threatening emergency
Death is rare when treatment is initiated
Results from stressors (infection, trauma, surgery)
Post-thyroidectomy patients at risk because of manipulation of the thyroid S/S
- Shock
- Severe tachycardia/HF
- Hyperthermia (106°F/41°C)
- Agitation
- Seizure
- GI pain, N/V, diarrhea
- Delirium, coma Monitor for dysrhythmias!!!! Iv fluid replacement, ensure adequate O2, give meds. Provide calm, quiet room, cool, light sheets
Block adverse effects of thyroid hormones
Suppress hormone oversecretion
Prevent complications
Medication and Treatments
Antithyroid hormone: First line antithyroids are propylthiouracil and methimazole (Tapazole). They inhibit synthesis of thyroid hormone. Improvement in 1-2 weeks. Best results in 4-8 weeks. Therapy for 6-15 months. Can be given to young Grave’s patients, pregnant women with hyperthyroidism, and needs for euthyroid prior to surgery or radiation.
Radioactive iodine therapy: Available as saturated solution of potassium iodine (SSKI) and Lugol's solution. Used with antithyroids to prepare for thyroidectomy or treatment of thyrotoxicosis. Maximal effect seen in 1-2 weeks. Long term iodine treatment is not effective. Iodine is mixed with juice or water, sipped on through a straw, given after meals. If iodine toxicity occurs, discontinue and call HCP.
B-Adrenergic Blockers: Sued for symptom relief of thyrotoxicosis. Blocks sympathetic nervous systems to decrease tachycardia, nervousness, irritability, and tremors. Propranolol given with antithyroids. Atenolol is preferred for those with asthma or heart disease.
Surgery (Subtotal thyroidectomy): Remove up to 90% of thyroid. Indicated for large goiter compressing trachea, unresponsive to anti-thyroids, thyroid cancer, not a candidate for RAI. helps with rapid reductions in T3 and T4 levels. Can be done minimally invasively. Post-op: risk for bleeding, airway compromised, electrolyte changes.
Exophthalmos: Artificial tears, salt restriction, elevated HOB, dark glasses, tape eyelids for sleep, ROM of intraocular muscles.
Disease: Hypothyroidism/Myxedema Coma
Pathophysiology Signs and Symptoms Diagnostic Tests
Deficiency of thyroid hormone. General metabolic slowing. Primary: Destruction of thyroid tissue, or defective hormone synthesis Secondary: Pituitary or hypothalamic dysfunction. (Decreased TSH or TSR)
Systemic slowing of body processes
Slow onset. Some might confuse for “normal aging”
Decreased cardiac output
Increased cholesterol and triglycerides
Anemia
Low exercise tolerance, SOB
Fatigue, lethargy, impaired memory, slowed speech, decreased initiative, somnolence.
Decreased appetite, N/V
Weight gain, constipation
Enlarged, scaly tongue
Celiac disease
Dry, thick, cold, inelastic skin
Thick, brittle nails
Dry, sparse, coarse hair
General interstitial edema
Puffy face
Decreased sweating, pallor
Prolonged periods or amenorrhea, decreased libido
Intolerance to cold
Sleepiness
Sensitivity to opioids, barbiturates and anesthesia.
Susceptible to infection
History and physical examination
Serum TSH and free T
Total serum T3 and T
Thyroid peroxidase (TPO) antibodies
Risk Factors Complications RN Interventions + Patient Teaching
- Women
- Iodine deficient
- Atrophy of the gland
- Treatment for hyperthyroidism
- Drugs
- Cretinism (hypothyroid in infancy)
Myxedema Coma: caused by stressor (infection, drugs, cold, trauma S/S: Impaired LOC, subnormal temperature, hypotension, hypoventilation. Cardiovascular collapse occurs due to hypoventilation, hyponatremia, hypoglycemia, and lactic acidosis.
- Treat with IV thyroid hormone.
- To survive, vital functions must be supported and hormones replaced ASAP.
Most only need outpatient therapy
Myxedema coma necessitates acute care: - Mechanical respiratory support - Cardiac monitoring - IV thyroid hormone replacement - Monitoring of core temperature
Medication and Treatments
Levothyroxine (Synthroid): Start with a low dose! - Monitor for CV effects (chest pain, dysrhythmias), weight loss, nervousness, tremors, insomnia - Increase dose in 4-6 week intervals as needed - Life long therapy
Disease: Lung Cancer
Pathophysiology Signs and Symptoms Diagnostic Tests
Primary lung cancers are categorized into 2 broad subtypes:
Non–small cell lung cancer (NSCLC) (85%)
Small cell lung cancer (SCLC) (15%).
Lung cancers metastasize primarily by direct extension and through the blood and lymph system. The common sites for metastasis are the lymph nodes, liver, brain, bones, and adrenal glands.
Anorexia/weight loss
Fatigue
N/V
Unilateral paralysis of the diaphragm
Dysphagia
Palpable lymph nodes (neck/axilla)
Hoarseness
Superior vena cava obstruction
Chest x-ray
CT
Sputum cytology: can identify malignant cells (not the best diagnostic)
Biopsy is required for a diagnosis (CT guided needle aspiration bronchoscopy, mediastinoscopy, or video assisted thoracoscopy)
Thoracentesis
Bone scans/CT scans assessing for metastasis
Complete hx and physical
CBC with diff
Chemistry panel
Liver function tests
Renal functions tests
Pulmonary function tests
MRI and PET may also be used to evaluate and stage cancer
Risk Factors Complications RN Interventions + Patient Teaching
Leading cause of cancer related deaths - Smoking - 2nd hand smoke exposure - Age - Pollution - Radiation - Asbestos - Heavy or prolonged exposure to industrial agents, such as ionizing radiation, coal dust, nickel, uranium, chromium, formaldehyde, and arsenic
Mediastinal involvement may lead to pericardial effusion, cardiac tamponade, and dysrhythmias.
- Provide patient comfort
- Teach methods to reduce pain
- Monitor for side effects of prescribed medications
- Foster appropriate coping strategies for the patient and caregiver
- Assess smoking cessation readiness
- Help patients to access resources to deal with the illness
Medication and Treatments
Surgical therapy: Resection gives the best chance for a cure. But many are not resectable at time of diagnosis. Radiation therapy: Radiation therapy may be given as curative therapy, palliative therapy (to relieve symptoms), or adjuvant therapy in combination with surgery, chemotherapy, or targeted therapy. Radiation is a primary option for those who cannot undergo surgical resection. Chemotherapy: Main treatment for SCLC. In NSCLC, chemotherapy may be used in the treatment of nonresectable tumors or as adjuvant therapy to surgery. Targeted therapy: Targeted therapy uses drugs that block the growth of molecules involved in specific aspects of tumor growth. Can be less toxic than chemo. Immunotherapy: Drugs that target PD-1, a protein on T cells that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth. Stereotactic radiotherapy
Disease: Acute Respiratory Failure (Hypoxemic)
Pathophysiology Signs and Symptoms Diagnostic Tests
Hypoxemic: Insufficient O2 transferred to blood.
Hypoxemic: Oxygenation failure PaO 2 ≤60 mmHg, on ≥60% oxygen - Acute= minutes - hours - Chronic= several days+
- Inadequate exchange of O 2 between the alveoli and pulmonary capillaries
- Dyspnea, tachypnea
- Prolonged expiration
- Use of accessory muscles
- Decreased SpO2 (<80%)
- Paradoxic chest
- Cyanosis
- Fatigue
- Inability to speak complete sentence w/o pausing for air CNS: confusion, agitation, disoriented, combative, delirium, decreased LOC, coma CV: tachycardia, HTN, cool/clammy/diaphoretic skin Dysrhythmias and hypotension (late)
Most common - Chest x-ray - ABG analysis/pulse oximetry Other - CBC, serum electrolytes, urinalysis - 12-lead ECG - Blood and sputum cultures - CT scan or V/Q scan - End tidal CO 2 (with mechanical ventilation)
Risk Factors Complications RN Interventions + Patient Teaching
Hypoxemic: Respiratory or cardiac disorders or disease (ABG= decreased PaO2 and SaO2)
- V/Q mismatch: occurs when ration is not 1:1 — COPD, pneumonia, asthma, pain, atelectasis, PE
- Shunting: occurs when blood goes through the heart bypassing the lungs or through the lungs bypassing the capillaries — Ventricular Septal defect, alveoli are filled with fluid (pneumonia)
- Diffusion limitation: Gas exchange in alveolar-capillary membrane is compromised — pulmonary fibrosis, interstitial lung disease, ARDS, pulmonary edema, hypoxemia with exercise
- Alveolar hypoventilation: Atelectasis — CNS conditions, chest wall disfunction, acute asthma, restrictive lung disease
Observe/Assess:
- Ability to speak — full or partial sentences, 2 to 3 word dyspnea
- Pursed-lip breathing Increased expiratory time; prevents small bronchial collapse
- Retraction of intercostal spaces or supraclavicular area; use of accessory muscles
- Paradoxical breathing — Abdomen and chest move opposite of normal
- Diaphoresis from # WOB
- Auscultate breath sounds — fine or coarse crackles, absent (consolidation), pleural rub Goals:
- Independently maintain a patent airway
- Absence of dyspnea or recovery to baseline breathing patterns
- Effectively cough and able to clear secretions
- Normal ABG values or values within patient's baseline
- Breath sounds within patient's baseline
Medication and Treatments
Hypoxemia: The first step to treat V/Q mismatch is O 2 therapy. Treat the underlying cause. O 2 therapy with mechanical ventilation and high FiO 2 may be needed. Reduce airway inflammation and bronchospasm — Corticosteroids and Bronchodilators Relieve pulmonary congestion — IV diuretics, Morphine, and Nitroglycerine Treat infections — IV antibiotics Reduce anxiety, pain, and restlessness — Benzodiazepines and Opioids *Never withhold O 2 from a hypoxic patient Maintain PaO 2 at 55 to 60 mm Hg or more and SaO 2 at 90% or more at the lowest O 2 concentration possible
Disease: Pneumothorax (Tension, Hemo, and Pneumo)
Pathophysiology Signs and Symptoms Diagnostic Tests
A pneumothorax is caused by air entering the pleural cavity. Normally, negative pressure exists between the visceral pleura (surrounding the lung) and parietal pleura (lining the chest cavity), known as the pleural space. When air enters this space, the change to positive pressure causes a partial or complete lung collapse Open: External wound Closed: No external wound
Small pneumothorax: mild tachycardia and dyspnea may be the only manifestations. Large area pneumothorax:
Respiratory distress
Short, shallow, rapid respirations
Dyspnea
Air hunger
O2 desaturation.
On auscultation, breath sounds are absent over the affected area.
A chest x-ray will show air or fluid in the pleural space and reduction in lung volume.
Tension Pneumothorax and Hemothorax/Hemopneumothorax
Tension Pneumothorax: Medical Emergency Occurs when air enters the pleural space but cannot escape. The continued accumulation of air in the pleural space causes increasingly elevated intrapleural pressures. This results in compression of the lung on the affected side and pressure on the heart and great vessels, pushing them away from the affected side. The mediastinum shifts toward the unaffected side, compressing the “good” lung, which further compromises oxygenation. As the pressure increases, venous return decreases and cardiac output falls.
- Tension pneumothorax can occur with mechanical ventilation and resuscitative efforts. It can also occur if chest tubes are clamped or become blocked in a patient with a pneumothorax. Unclamping the tube or relieving the obstruction may correct this situation.
- S/S: Severe dyspnea, tachycardia, tracheal deviation, decreased/absent breath sounds on the affected side, neck vein distention, cyanosis, and profuse diaphoresis.
- Patient will likely die if the tension in the pleural space is not relieved, due to inadequate cardiac output or severe hypoxemia. Hemothorax/Hemopneumothorax: An accumulation of blood in the pleural space from injury to the chest wall, diaphragm, lung, blood vessels, or mediastinum. When it occurs with pneumothorax, it is called a hemopneumothorax. The patient with a traumatic hemothorax needs immediate insertion of a chest tube for evacuation of the blood. Recovered blood can be reinfused for a short time after the injury (Autotransfusion: blood circulated back into the body)
Medication and Treatments
- If the patient is stable and has minimal air and/or fluid accumulated in the intrapleural space, no treatment may be needed since the condition may resolve spontaneously.
- Emergency treatment consists of covering the wound with an occlusive dressing that is secured on 3 sides (vent dressing). During inspiration, as negative pressure is created in the chest, the dressing pulls against the wound, preventing air from entering the pleural space. During expiration, as the pressure rises in the pleural space, the dressing is pushed out and air escapes through the wound and from under the dressing.
- The most definitive and common treatment of pneumothorax and hemothorax is to insert a chest tube and connect it to water-seal drainage.
- Repeated spontaneous pneumothorax may need surgical treatment with a partial pleurectomy, stapling, or pleurodesis to promote adherence of the pleurae to one another.
- Tension pneumothorax is a medical emergency, requiring urgent needle decompression followed by chest tube insertion to water-seal drainage.
Disease: Status Asthmaticus
Pathophysiology Signs and Symptoms Diagnostic Tests
Recurrent episodes of wheezing, breathlessness, coughing, and tight chest
Triggers: allergens, exercise, URI, foods, emotions, NSAIDs, Beta blockers, ACEI
Use of accessory muscles
Diaphoresis
Cyanosis
Detailed hx and physical
Spirometry
Peak expiratory flow rate (PEFR)
Chest x-ray
ABGs, CBC, CMP, Pulse ox, cultures to rule out infection
In a patient asthma plan, are they in the red zone?
Risk Factors Complications RN Interventions + Patient Teaching
Severe and life-threatening exacerbations
- RR >30/min
- Dyspnea at rest
- Pulse >
- PEFR is 40% at rest
- Usually an ED visit or hospitalization Life-threatening exacerbations
- Too dyspneic to speak
- Perspiring profusely
- Drowsy/confused
- PEFR<25%
- Often admitted to the ICU
- “Silent chest”
- Requires ED and possible ICU
- IV magnesium sulfate
- 100% oxygen
- Hourly or continuous nebulized SABA
- IV corticosteroids
- PEFR= peak expiratory flow rate
- Assess RR and HR
- Use of accessory muscles
- Percussion (hyperresonance)and auscultation of lungs
- PERF to monitor airflow
- ABGs and pulse ox
- Give O 2 via nasal cannula
- Achieve a PaO 2 of ≥60 mmhg or SpO 2 of 90%
- Continuous O 2 monitoring
- Treat with bronchodilator
Medication and Treatments
Corticosteroids: IV or inhaled — first-line therapy for patients with persistent asthma (1-2 week use before maximum effects to be seen — flovent works in 24 hours) Bronchodilators: SABA and LABA Anticholinergic drugs
Explore-More Notes
Rapid response teams
Palliative and EOL care
Management of ventilated patients: (p. 1553)
Air is moved in and out of the lungs through the work of a machine
Positive pressure ventilations: Fixed rate of air, and fixed pressure. Usually used for ARDs.
Negative pressure ventilation: Creates a negative pressure environment, allows for passive expiration.
Nursing priorities
- O 2 tox
- Watch oxygenation and ventilation
- Manage mechanical setting
- Skin breakdown
- Moving tube to prevent pressure ulcers
- Suctioning
- Oral care
- No kinks in the tubing
- Prone position is important! Allows for full lung expansion dn shift of fluids in the lungs
- Q2 turning
- Prevent tube dislodgement, may need soft restraints. Ventilator-Associated Pneumonia (VAP): What is it? How can we prevent it?
Sedation vacations
Hand hygiene
HOB at 30
Wear gloves
Oral care with chlorhexidine
Q2 turning
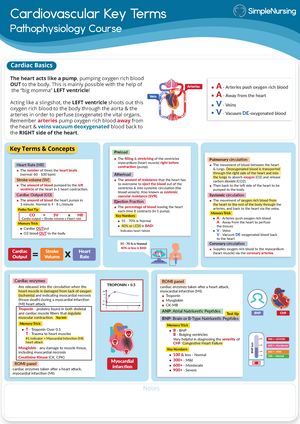
Fluid and electrolyte balance: - Potassium imbalances: - Heart complications - Keep balanced with IV and oral supplementation - Continuous ECG monitoring
Hypertonic Fluids (3% and 5% NS): - Sodium concentration is higher than what is in the blood. - Hyponatremia due to SIADH - Use this to not fluid overload these patients
Hypotonic fluids (0% NS) - Use in DKA, HHS, DI - Rehydrate without overloading with sodium Isotonic fluids (0% NS, and LR):
- Best for DKA
- N/V/D
ABGs and compensation
Chest trauma (blunt, flail, chest tubes, thoracotomy, lung transplant)
ARDs
Hemodynamic monitoring - Noninvasive: Vital signs - Invasive: Arterial lines — things measured by art lines: - Maintaining MAP above 60 - Central venous pressure (CVP)
Corticosteroid Therapy: - Effective in treating many disorders - Take in the morning with food - Complications arise with long term use, not recommended for minor chronic conditions. - For use, potential benefits must outweigh risks - Expected outcomes: Antiinflammatory, immunosuppression, maintenance of normal BP (has vasopressive effects) - Side effects: Hypokalemia, hypocalcemia, increased BG and BP, delayed wound healing, susceptible to infection, PUD, muscle wasting, mood changes, moon face, truncal obesity, protein depletion, risk for acute adrenal crisis if stopped abruptly - Patient teaching: - High protein, high calcium, high potassium diet. - Low fat, low sugar, low simple carbohydrates. - Develop an exercise program for muscle and bone integrity. - For osteoporosis prevention, take calcium, vitamin D, and bisphosphonates. - <2000 mg/day of sodium if edema occurs. - Monitor BG for hyperglycemia - Yearly eye checks (cataracts) - Notify HPC of epigastric pain or heartburn not relieved by antacid - Use good hygiene, avoid crowds and contact with contagious illness
● Addisonian Crisis
430 Exam 1 Study Guide
Course: Adult Health Nursing II (NSG-430)
University: Grand Canyon University

- Discover more from: