- Information
- AI Chat
Exam 1 Study Guide
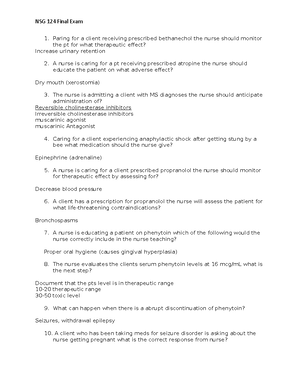
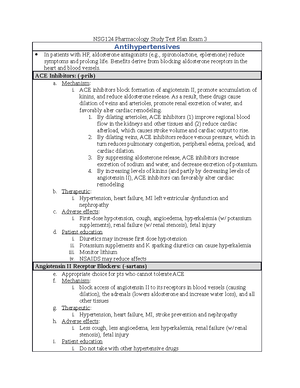
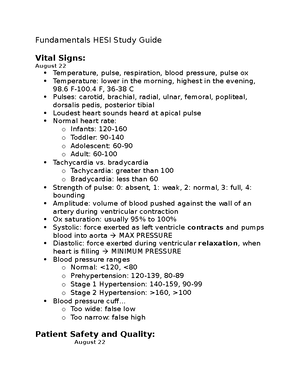
Pharmacology (NSG 124)
Herzing University
Recommended for you
Preview text
UNIT ONE
Assessing Pain and Pain Management Defining goals Identifying interventions Evaluating success
Drug Names Generic Less complex, only one name per drug Nonproprietary Suffixes Drug name not capitalized Example - acetaminophen Trade Name under which the drug is marketed Multiple trade names Proprietary Drug name is capitalized Example - Tylenol Chemical The 1st name that a drug is given Constitutes a description of a drug using the nomenclature of chemistry Inappropriate for everyday use
Over the Counter Medications Same name with different active ingredients No significant differences that exist between brand and generic; however, there are a few generic drugs that have a slight increase in absorption which can result in toxicity or a slight decrease in the medication with results in therapeutic failure Assessment Education
Drug-Food Interactions Impact on food-drug interactions: Decreased absorption Food frequently decreases the rate of drug absorption and occasionally decreases the extent of absorption The interaction between calcium-containing foods and tetracycline is a classic example High-fiber foods can reduce absorption of drugs Increased absorption When this occurs, peak effects are heightened High-calorie meals can increase absorption Grapefruit juice effect
Raises drug levels in the blood stream Intestinal metabolism IV medication is not affected by grapefruit juice
Major Pharmacokinetics Processes 4 phases of drug movement: Medication absorption Rate of dissolution Meaning it must first be dissolved Influenced by the physical and chemical properties of the drug itself and by physiologic and anatomic factors at the absorption site Absorption is defined as the movement of a drug from its site of administration into the blood The larger the surface area, the faster it will be absorbed Drug flows more rapidly when blood flow is high Lipid solubility more rapid with high lipid soluble products Lipid soluble drugs can readily cross the membranes that separate them from the blood pH partitioning happens when there is a difference between the pH of the plasma and the pH at the site of administration (absorption will be enhanced) Medication distribution Blood flow to the tissues Carried by the blood to the tissues and organs Abscesses and tumors can affect blood flow Exiting the vascular system Typical capillary beds No resistance to the departure of the drug meaning that drugs can pass freely in and out of the bloodstream Blood brain barrier Only drugs that are lipid soluble or have a transport system can cross the BBB to a significant degree In addition to tight junctions, the BBB uses P-glycoprotein as a protective component Placenta drug transfer Lipid-soluble, nonionized compounds readily pass from the maternal bloodstream into the blood of the fetus Compounds that are ionized, highly polar, or protein bound are largely excluded Protein binding Allows for the medication to attach to a protein molecule such as albumin, the disadvantage to this process is that the protein binding sites are limited and drugs compete for the protein molecules, which causes a free concentration of the displaced drug to rise resulting in a possible toxicity
pH dependent ionization Competition for active tubular transport Age Kidney disease Assessment and evaluation
Drug Levels and Half Life Half-life is defined as the time required for the amount of the drug in the body to be decreased by 50% Determines dosing interval Long half-life is preferred due to dosing First-pass effect Renal medication excretion Therapeutic index Narrow therapeutic Can be difficult to manage Wide therapeutic Safer to administer Toxic levels Too much of a drug Nontherapeutic level Too little of the drug
Drug to Drug Interactions Adverse effects Consequences: Intensification of effects – good or bad Reduction of effects – therapeutic or adverse Creation of unique response Therapeutic effects The creation of a unique response can be seen in when a medication combines with another medication or substance to give a result that is not seen when using the medication alone Rarely, the combination of two drugs produces a new response not seen with either agent alone Enhance or decrease effects Intensification of effects is when one drug intensifies the effects of another drug The increase in adverse effects is not one we want our patients to experience Reduction of effects is defined as inhibitory interactions that reduce toxicity Reduced therapeutic effects Reduced adverse effects Mechanism of drug-drug interactions Direct chemical or physical interactions
Pharmacokinetics interactions Pharmacodynamic interactions Combined toxicity
Toxicities and Assessment Skills Adverse reactions Side effects A nearly unavoidable secondary drug effect produced at therapeutic doses May develop soon after drug is initiated or not until drug has been taken for weeks or months Can include a variety of symptoms – may not be a true allergy Toxicity Formal definition – adverse drug reaction caused by excessive dosing May occur even with normal dosing Allergic reaction Immune response Determined primarily by the degree of sensitization of the immune system rather than by drug dosage Patient’s sensitivity to a drug can change over time Very few drugs cause severe allergic reactions Penicillins are the most common Allergies may also be induced by sulfonamides Idiosyncratic effect An uncommon drug response resulting from a genetic predisposition Patient with different genetic deficiency can have this effect Can be life threatening Paradoxical effect Opposite effect than the intended effect Example – diphenhydramine can cause some patients to have excitability versus a sedative effect Iatrogenic disease An iatrogenic disease is a disease that occurs as a result of medical care or treatment Can also be used to denote a disease produced by drugs Physical dependence Physical dependence is a state in which the body has adapted to drug exposure in such a way that an abstinence syndrome will result if drug use is discontinued The precise nature of the abstinence syndrome is determined by drug involved Develops during long-term use of certain drugs, such as opioids, alcohol, barbiturates, and amphetamines Carcinogenic effect
Types of errors Human Wrong patient Wrong drug Wrong route Wrong time Wrong dose Wrong dosage form Wrong diluent Communication Name confusion
Factors Influencing Medication Response Age Drug sensitivity varies with age Infants resulting from organ immaturity Older adult’s organs decline in function Tolerance Tolerance is a decreased responsiveness to a drug because of repeated drug administration Patients who are tolerant to a drug require higher doses to produce effects equivalent to those that could be achieved with lower doses before tolerance developed Three categories of drug tolerance: Pharmacodynamic tolerance Metabolic tolerance Tachyphylaxis Body weight and composition Body size can be a significant determinant of drug effects The higher the concentration, the more intense the response Adjusting the dosage to account for body weight
Drug Therapy and Pregnancy and Pediatrics Basic considerations Adverse reactions Teratogens Birth defects/Congenital anomalies Gross malformations Cleft palate, clubfoot, and hydrocephalus Neurobehavioral and metabolic anomalies Incidence and cause of congenital anomalies Less than 1% of all birth defects caused by drugs Identification of teratogens very difficult Occurs in the 1st trimester Results in gross formation and loss of function FDA pregnancy risk categories
Drug Therapy for Older Adults & End of Life Pharmacokinetic changes in older adults
Drugs for Muscle Spasm & Pain Baclofen Helps to relieve spasms due to MS or spinal cord injuries No direct muscle-relaxant action Mechanism of action Acts within the spinal cord to suppress hyperactive reflexes involved in the regulation of muscle movement Therapeutic use Baclofen can reduce spasticity associated with MS and spinal cord injury The drug decreases flexor and extensor spasms and suppresses resistance to passive movement These actions reduce the discomfort of spasticity and allow increased performance Short half-life – 4 to 4 hours Adverse effects – GI: nausea, vomiting, constipation, urinary retention CNS: drowsiness, dizziness, fatigue, and weakness Withdrawal Symptoms when stopped – paranoid ideations, seizures, visual hallucination Always taper down medications Cyclobenzaprine Mechanism of action Centrally acting skeletal muscle relaxant Activity takes place primarily in the brainstem and results in a reduction of tonic motor activity Therapeutic use Used for the relief of muscle spasms and associated pain Considered the most efficacious of the drugs used for this purpose First choice for acute muscle spasms; ineffective as a treatment for spasticity Adverse effects CNS – drowsiness, dizziness, and fatigue Anticholinergic effects – dry mouth, blurred vision, photophobia, urinary retention, constipation Irregular rhythms – tachycardia Contraindications and interactions MAOIs and cyclobenzaprine can cause serotonin syndrome Alcohol and other CNS depressants Causes additive CNS depression
Facilitate other procedures Agents used: Induction of anesthesia – propofol and short-acting barbiturates Muscle relaxation – neuromuscular blocking agents Analgesia – opioids and nitrous oxide The combination of medications allows for a small, safer dose of the inhaled anesthetic Adverse effects – Respiratory and cardiac depression Malignant hyperthermia
Nursing Care: Local & General Anesthetics – Topical, Injectable, and Inhalation Pre-assessment Prior to giving the medication, you will need to assess the patient including pain level, vital signs, and level of consciousness Address baseline CNS Take high risk patients into consideration Note the age of the patient Administration Routes PO, sublingual, IM, IV, subq, transdermal, and rectal suppositories Dosage Will vary depending on the department you are working in Any time you give a narcotic IV, you must administer slowly Ongoing evaluation and interventions Minimizing adverse effects Respiratory depression Sedation Orthostatic hypotension Constipation Urinary retention Biliary colic Emesis Cough suppression Miosis Neurotoxicity Birth defects Opioid dependence Dysrhythmias
Opioid Antagonist Agents Classification of opioids Pharmacologic action Therapeutic use
Mechanism of action Adverse effects
Opioid Nursing Considerations Pre-administration assessment Administration Evaluations and interventions
Opioid Antagonists Naloxone (Narcan) Used to reverse opioid agonist Mechanism of action Pharmacologic effects Pharmacokinetics Therapeutic uses Reversal of respiratory and central nervous system depression caused by overdose with opioid agonists Prep, dose, and administration Route – IV, IM, inhaled, subcutaneous Nursing considerations: LOC Vital signs Safety
UNIT TWO Migraine Treatment Agents & Nursing Considerations Mild to moderate Aspirin like drugs Opioid analgesic Moderate to severe Serotonin agonist Ergot alkaloid alters serotonin Serotonin1B/1D receptor agonists Mechanism of action Binds to receptors on intracranial blood vessels and causes vasoconstriction Diminishes perivascular inflammation Therapeutic use Pharmacokinetics Adverse effects Vertigo, malaise, fatigue, and tingling sensations Very bad taste when taken in intranasal form Drug interactions
Histamine Agents and Nursing Considerations Two types of histamines
Inhibits cyclooxygenase and has anti-inflammatory, analgesic, and antipyretic actions Pharmacokinetics Cyclooxygenase-1 (COX-1) produces prostaglandins that stimulate gastric mucous production, enhance renal perfusion, and assist platelets to form clots Cyclooxygenase-2 (COX-2) produces prostaglandins that perpetuate inflammation; cause pain, fever, swelling, muscle contractions; and potentiate effects of other inflammatory mediators Therapeutic uses Used to treat inflammatory disorders (RA, osteoarthritis, bursitis) Alleviate mild to moderate pain Suppress fever Relieve dysmenorrhea Suppress inflammation but pose risk of serious harm Adverse effects First generation Low incidence of adverse effects Second generation Dyspepsia Abdominal pain Renal impairment Sulfonamide allergy Cardiovascular impact Use in pregnancy Expected effects Reduction of fever and mild to moderate pain
Acetaminophen Action and Effects Mechanism of action Inhibits prostaglandin synthesis in central nervous system Pharmacokinetics Adverse effects Very few at normal doses Liver damage with overdose Increased risk for hypertension and asthma for patients who use acetaminophen daily Steven-Johnson syndrome, acute generalized exanthematous pustulosis, and toxic epidermal necrolysis Therapeutic uses Analgesic, antipyretic Does not technically have any anti-inflammatory or antirheumatic actions Not associated with Reye’s syndrome Drug and vaccine interactions
Acute toxicity Acetylcysteine is used to prevent liver damage in an overdose of acetaminophen
Nursing Considerations of Aspirin All benefits result from inhibiting COX-2, except for prevention of MI or stroke which results from inhibiting COX- Aspirin inhibits both COX-1 and COX- Poses risk for gastric ulcers, bleeding, and renal impairment Therapeutic goal Analgesic, antipyretic, anti-inflammatory Suppression of platelet aggregation Protects in thrombotic disorders Dysmenorrhea Cancer prevention Prevention of Alzheimer’s disease Adverse effects GI effects Bleeding Renal impairment Salicylism Reye’s syndrome Pregnancy Hypersensitivity reaction Interactions With alcohol – it will thin out blood Minimizing adverse interactions Patient education: Stop taking prior to surgeries or procedures Nursing considerations: Educate the patient about what it is being used for Monitor for bruising or signs/symptoms for bleeding Monitor kidney functions – BUN, creatinine, GFR
Nursing Care for Glucocorticoids Major nursing implications Uses – Physiologic – modulation of glucose metabolism (low doses) Pharmacologic – suppression of inflammation and immune responses (high doses) Used to treat nonendocrine disorders such as arthritis, asthma, cancer, or suppression of allograft rejection Commonly added to regimen when acute respiratory disease occurs Pre-administration assessment Assess high risk patients:
Mucolytics – things the mucus to allow the cough to be more productive Analgesic – pain medications Antihistamine Caffeine
Peptic Ulcer Agent Action, Effects, and Pharmacokinetics Antibiotic drugs Used when patient has a confirmed infection of H. pylori Most patients will be on the medication for 10 to 14 days and probably will experience bouts of diarrhea Histamine 2 receptor antagonist Blocks H2 receptors reducing both the volume of gastric juice and its hydrogen ion concentration First choice drugs for treating gastric and duodenal ulcers Promote healing by suppressing secretion of gastric acids Serious side effects are uncommon Uses: GERD Aspiration pneumonia Heartburn and acid indigestion Adverse effects: Antiandrogen effects CNS effects Pneumonia Proton pump inhibitors Used for gastric and duodenal ulcers and GERD Most effective drugs for suppressing secretion of gastric acid Therapeutic use – short term Gastric/duodenal ulcers GERD Selection of PPI is based on cost and prescriber’s preference Protonix Used to treat GI bleeds, patients who have a GI bleed will be on a protonix drip to help suppress the gastric juices Adverse effects – Pneumonia Fractures Hypomagnesemia Rebound acid hypersecretion Mechanism of action Pharmacokinetics Therapeutic uses Adverse effects Prep, dose, and administration
Nursing Care for Peptic Ulcer Agents H2 receptor antagonists & proton Pre-administration assessment Administration Measure to enhance therapeutic effects Evaluation and intervention
Drugs and Nursing Considerations for Constipations Classifications of laxatives by category Bulk forming Mechanism of action Have impact on bowel function as dietary fiber Swell in H 2 O to form a viscous solution or gel, softening the fecal mass and increasing its bulk Indications Temporary relief of constipation Widely used in patients with diverticulosis and IBS Can provide symptomatic relief of diarrhea Can reduce discomfort and inconvenience for patients with an ileostomy or colostomy Adverse effects Esophageal obstruction if not given with a full glass of H 2 O Intestinal obstruction or impaction if intestine is impeded Surfactant laxatives Mechanism of action Lowers surface tension, which facilitates penetration of fluid into the feces Dosage forms Capsules Tablets Syrup Liquid Stimulant laxatives Mechanism of action Stimulate intestinal motility Increase the amount of H 2 O and electrolytes in the intestinal lumen Osmotic laxatives Mechanism of action Draws water into the intestinal lumen Uses To empty the bowel in preparation for diagnostic and surgical procedures Adverse effects Dehydration Can exacerbate heart failure, hypertension, and edema
Prolonged duration of action Adverse effects: Generally well tolerated Motion sickness drugs Motion sickness is caused by air, sea, automobile, and space travel Symptoms include nausea, vomiting, pallor, and cold sweats Treatment: Scopolamine Suppresses the nerves from the inner ear that lead to the vomiting center Adverse effects Dry mouth Blurred vision Drowsiness Urinary retention/constipation Disorientation Antihistamines Inhibits nerves from the inner ear to the vomiting center Side effects Dry mouth Blurred vision Sedation Constipation Antidiarrheal drugs Defines as a symptom of a GI disease, not a disease itself Management is aimed at: Diagnosis and treatment of underlying cause Replacement of lost water and salts Relief of cramping Reducing the passage of unformed stools Drug categories: Specific antidiarrheal drugs Opioids Diphenoxylate Loperamide Nonspecific antidiarrheal drugs
Other GI Agents for Irritable and Inflammatory Bowel Drugs for irritable bowel Drugs for inflammatory bowel Prokinetic agents Action Therapeutic uses Adverse effects
Antiemetics, Motion Sickness Drugs & Antidiarrheals
Actions Therapeutic use Pharmacokinetics Adverse effects Drug interactions
Exam 1 Study Guide
Course: Pharmacology (NSG 124)
University: Herzing University

- Discover more from: