- Information
- AI Chat
EXAM 3 Study Guide Pharmacology
Pharmacology (NSG 124)
Herzing University
Recommended for you
Related Studylists
Information for BSN programPreview text
EXAM 3 STUDY GUIDE
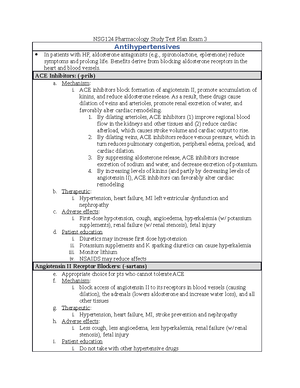
Module 9 & 10 1. RAA Drugs: Therapeutic Effects/ Adverse Effects - ACE Inhibitors, Therapeutic Effects: All ACE inhibitors are approved for hypertension. - ACE inhibitors produce multiple benefits in heart failure. o By lowering arteriolar tone, these drugs improve regional blood flow, and by reducing cardiac afterload, they increase cardiac output. o By causing venous dilation, they reduce pulmonary congestion and peripheral edema. By dilating blood vessels in the kidney, they increase renal blood flow and thereby promote excretion of sodium and water. o By suppressing aldosterone and reducing local production of angiotensin II in the heart, ACE inhibitors may prevent or reverse pathologic changes in cardiac structure. - ACE inhibitors can reduce mortality following acute MI (heart attack). In addition, they decrease the chance of developing overt heart failure. o At this time, only three ACE inhibitors—captopril, lisinopril, and trandolapril—are approved for patients with MI. - ACE inhibitors can benefit patients with diabetic nephropathy o ACE inhibitors can slow progression of renal disease o ACE inhibitors can delay onset of overt nephropathy o The principal protective mechanism appears to be the reduction of glomerular filtration pressure. - One ACE inhibitor (ramipril [Altace]) is approved for reducing the risk of MI, stroke, and death from cardiovascular causes in patients at high risk for a major cardiovascular - Adverse Effects: A precipitous drop in blood pressure may occur following the first dose of an ACE inhibitor o First-dose hypotension is most likely in patients with severe hypertension, in patients taking diuretics, and in patients who are sodium depleted or volume depleted. - All ACE inhibitors can cause persistent dry, irritating, nonproductive cough. o The underlying cause is accumulation of bradykinin secondary to inhibition of kinase II (another name for ACE). - Inhibition of aldosterone release (secondary to inhibition of angiotensin II production) can cause potassium retention by the kidney o Patients should be instructed to avoid potassium supplements and potassium-containing salt substitutes unless they are prescribed. o Although in most cases hyperkalemia is rare - ACE inhibitors can cause severe renal insufficiency in patients with bilateral renal artery stenosis or stenosis in the artery to a single remaining kidney. - For a long time, it has been known that use of ACE inhibitors during the second and third trimesters of pregnancy can injure the developing fetus. o Specific effects include hypotension, hyperkalemia, skull hypoplasia, pulmonary hypoplasia, anuria, renal failure (reversible and irreversible), and death - Angioedema is a potentially fatal reaction that develops in up to 1% of patients. o Symptoms, which result from increased capillary permeability, include giant wheals and edema of the tongue, glottis, lips, eyes, and pharynx o Angioedema is caused by accumulation of bradykinin secondary to inhibition of kinase II. - Neutropenia, with its associated risk of infection, is a rare but serious complication o neutropenia may progress to fatal agranulocytosis. - ARBs: All ARBs are approved for hypertension. o Reductions in blood pressure equal those seen with ACE inhibitors.
o Whether ARBs share the ability of ACE inhibitors to reduce mortality has not been established.
- Currently, only two ARBs—valsartan [Diovan] and candesartan [Atacand]—are approved for heart failure
- Two ARBs—irbesartan [Avapro] and losartan [Cozaar]—are approved for managing nephropathy in hypertensive patients with type 2 diabetes. o As noted previously, neither ARBs nor ACE inhibitors are effective for primary prevention of diabetic nephropathy.
- One ARB—valsartan [Diovan]—is approved for reducing cardiovascular mortality in post-MI patients with heart failure or LV dysfunction
- One ARB—losartan [Cozaar]—is approved for reducing the risk of stroke in patients with hypertension and LV hypertrophy.
- One ARB—telmisartan [Micardis]—is approved for reducing the risk of MI, stroke, and death from cardiovascular causes in patients age 55 years and older, but only if they are intolerant of ACE inhibitors.
- Adverse Effects: ARBs can cause angioedema, although the incidence may be lower with ARBs.
- Like the ACE inhibitors, ARBs can injure the developing fetus if taken during the second or third trimester of pregnancy
- ARBs can cause renal failure in patients with bilateral renal artery stenosis or stenosis in the artery to a single remaining kidney.
- Aldosterone Antagonists: Aldosterone antagonists are drugs that block receptors for aldosterone. o Two such agents are available: eplerenone and spironolactone
- Nursing Care for RAA Drugs: Identifying High Risk Patients/ Minimizing Adverse Effects
- ACE Inhibitors, Identifying High Risk Patients: ACE inhibitors are contraindicated during the second and third trimesters of pregnancy and for patients with o bilateral renal artery stenosis (or stenosis in the artery to a single remaining kidney) o a history of hypersensitivity reactions (especially angioedema) to ACE inhibitors.
- Exercise caution in patients with salt or volume depletion, renal impairment, or collagen vascular disease, and in those taking potassium supplements, salt substitutes, potassium-sparing diuretics, ARBs, aliskiren, or lithium.
- Minimizing Adverse Effects: Severe hypotension can occur with the first dose. o Minimize hypotension by withdrawing diuretics 2 to 3 days before initiating ACE inhibitors Using low initial doses. o Monitor blood pressure for 2 hours following the first dose. o Instruct patients to lie down if hypotension develops. If necessary, infuse normal saline to restore pressure.
- Sometimes your blood pressure drops momentarily and is most likely to occur when you start a medication, increase dosage, or even just stand up suddenly from a sitting or lying position. o This can be prevented or decreased by moving to a standing position slowly, sleeping with the head of the bed elevated, wearing elastic stockings, exercising legs, avoiding prolonged standing, and avoiding hot baths. o If episodes still occur, you should sit or lie down to avoid a fall and possible injury. Discuss persistent dizziness with your prescriber; this may indicate a need for changing the timing or type of medication.
- Warn patients about the possibility of persistent dry, irritating, nonproductive cough. o Instruct them to consult the prescriber if cough is bothersome.
- ACE inhibitors may increase potassium levels. o Instruct patients to avoid potassium supplements and potassium-containing salt substitutes unless they are prescribed by the provider.
o Exercise caution in patients taking an ACE inhibitor.
- Warn women of childbearing age that aliskiren taken during the second and third trimesters of pregnancy can cause fetal injury (hypotension, hyperkalemia, skull hypoplasia, anuria, reversible and irreversible renal failure, death). o If the patient becomes pregnant, withdraw aliskiren as soon as possible. o Closely monitor infants who have been exposed to aliskiren during the second or third trimester for hypotension, oliguria, and hyperkalemia.
- Angioedema is a rare and potentially fatal reaction is characterized by giant wheals and edema of the tongue, glottis, and pharynx. o Instruct patients to seek immediate medical attention if these symptoms develop. o If angioedema is diagnosed, aliskiren should be discontinued and never used again. Treat severe reactions with subcutaneous epinephrine.
- Nursing Care for Calcium Channel Blockers: Ongoing Evaluations and Interventions/ Minimizing Adverse effects/ Minimizing Adverse Reactions
- Verapamil and Diltiazem and Dihydropyridines, Ongoing Evaluations and Interventions: Keep an ongoing record of anginal attacks, noting the time and intensity of each attack and the likely precipitating event. o Teach outpatients to chart the time, intensity, and circumstances of their attacks and to notify the prescriber if attacks increase.
- Monitor blood pressure periodically. o For most patients, the goal is to reduce systolic/diastolic pressure to a value below 140/90 mm Hg. o Teach patients to self-monitor their blood pressure and to maintain a blood pressure record.
- Minimizing Adverse Effects: Verapamil and diltiazem can cause bradycardia, AV block, and heart failure. o Inform patients about manifestations of cardiac effects and instruct them to notify the prescriber if these occur.
- Inform patients about signs of edema (swelling in ankles or feet), and instruct them to notify the prescriber if these occur. o If necessary, edema can be reduced with a diuretic.
- Constipation occurs primarily with verapamil. o Advise patients that constipation can be minimized by increasing dietary fluid and fiber.
- Minimizing Adverse Interactions: The combination of digoxin with verapamil or diltiazem increases the risk of partial or complete AV block. o Monitor for indications of impaired AV conduction (missed beats, slowed ventricular rate). o Verapamil (and possibly diltiazem) can increase plasma levels of digoxin. Digoxin dosage should be reduced.
- Concurrent use of a beta blocker with verapamil or diltiazem can cause bradycardia, AV block, or heart failure. o Monitor closely for cardiac suppression. o Administer intravenous verapamil and beta blockers several hours apart.
- Grapefruit juice can raise levels of verapamil and diltiazem. o Advise patients that it may be prudent to minimize grapefruit juice consumption.
- Calcium channel blocker (CCB) overdose is often lethal. o Conventional medical treatment includes IV calcium, high doses of catecholamines, insulin, and glucagon. o A new inotropic drug, levosimendan, should be considered in severe CCB poisoning. o Remove unabsorbed drug with gastric lavage followed by activated charcoal.
Give IV calcium to help counteract excessive vasodilation and reduced myocardial contractility. o To raise blood pressure, give IV norepinephrine. Intravenous fluids and placing the patient in modified Trendelenburg's position can also help. o Bradycardia and AV block can be reversed with atropine and glucagon. If these are inadequate, electronic pacing may be required.
- Dihydropyridines Adverse Effects: Reflex tachycardia can be suppressed with a beta blocker.
- Vasodilator Agents: Overview of Therapeutic Uses/ Adverse Effects Related to Vasodilation/ Therapeutic uses/ Adverse Effects
Overview of Therapeutic uses: Principal indications are essential hypertension, hypertensive crisis, angina pectoris, heart failure, and myocardial infarction. o Additional indications include pheochromocytoma, peripheral vascular disease, pulmonary arterial hypertension, and production of controlled hypotension during surgery.
Adverse Effects Related to Vasodilation: Vasodilators place patients at increased risk of falls. o Patients receiving vasodilators should be informed about symptoms of hypotension (light- headedness, dizziness) and advised to sit or lie down if these occur.
Reflex tachycardia can be produced by dilation of arterioles or veins. The mechanism is this: o arteriolar dilation causes a direct decrease in arterial pressure or o venous dilation reduces cardiac output, which in turn reduces arterial pressure o baroreceptors in the aortic arch and carotid sinus sense the drop in pressure and relay this information to the vasomotor center of the medulla o in an attempt to bring blood pressure back up, the medulla sends impulses along sympathetic nerves instructing the heart to beat faster.
To help prevent vasodilator-induced reflex tachycardia, patients can be pretreated with a beta blocker (e., metoprolol), which will block sympathetic stimulation of the heart.
Prolonged use of arteriolar or venous dilators can cause an increase in blood volume (secondary to prolonged reduction of blood pressure). o First, reduced blood pressure triggers secretion of aldosterone by the adrenal glands. Aldosterone then acts on the kidney to promote retention of sodium and water, thereby increasing blood volume. o Second, by reducing arterial pressure, vasodilators decrease both renal blood flow and glomerular filtration rate; because filtrate volume is decreased, the kidney is able to reabsorb an increased fraction of filtered sodium and water, which causes blood volume to expand. Increased blood volume can negate the beneficial effects of the vasodilator.
To prevent the kidney from neutralizing the beneficial effects of vasodilation, patients often receive concurrent therapy with a diuretic, which prevents fluid retention and volume expansion.
Nitroprusside: is used to lower blood pressure rapidly in hypertensive emergencies. o Oral antihypertensive medication should be initiated simultaneously. o During nitroprusside treatment, furosemide may be needed to prevent excessive retention of fluid. o Nitroprusside is approved for producing controlled hypotension during surgery (to reduce bleeding in the surgical field) and for acute decompensated heart failure. o The drug has been employed investigationally to treat myocardial infarction.
Adverse Effects: If administered too rapidly, nitroprusside can cause a precipitous drop in blood pressure, resulting in headache, palpitations, nausea, vomiting, and sweating. o Blood pressure should be monitored continuously.
Rarely, lethal amounts of cyanide have accumulated.
Encourage patients to adopt a diet rich in fruits, vegetables, and low-fat dairy products and low in total fat, unsaturated fat, and cholesterol.
Encourage patients to limit alcohol consumption to 1 ounce/day (for most men) and 0 ounce/day (for women and lighter weight men). o One ounce of ethanol is equivalent to about two mixed drinks, two glasses of wine, or two cans of beer.
Encourage patients with a sedentary lifestyle to perform 30 to 45 minutes of aerobic exercise (e., walking, swimming, bicycling) most days of the week.
Strongly encourage patients to quit smoking. o Teach patients about aids for smoking cessation (e., nicotine patch, bupropion, varenicline).
- Nursing Care for Antidysrhythmic Agents: Quinidine, Lidocaine, Amiodarone/ Therapeutic goal/ Administration/ Pre-administration assessment/ Ongoing evaluation and interventions
- Quinidine: The usual goal is long-term suppression of atrial and ventricular dysrhythmias.
- Obtain a baseline ECG and laboratory evaluation of liver function. o Determine blood pressure. o Quinidine is contraindicated for patients with a history of hypersensitivity to quinidine or other cinchona alkaloids and for patients with complete heart block, digoxin toxicity, or conduction disturbances associated with marked QRS widening and QT prolongation. o Exercise caution in patients with partial AV block, HF, hypotensive states, and hepatic dysfunction.
- Administration is mainly oral, rarely IM or IV. o Advise patients to take quinidine with meals. Warn them not to crush or chew sustained-release formulations. o Dosage size depends on the particular quinidine salt being used: 200 mg of quinidine sulfate is equivalent to 275 mg of quinidine gluconate.
- Monitor for beneficial changes in the ECG. o Plasma drug levels should be kept between 2 and 5 mcg/mL.
- Diarrhea and other GI disturbances occur in one-third of patients and frequently force drug withdrawal. o Inform patients that they can reduce GI effects by taking quinidine with meals.
- Inform patients about symptoms of cinchonism (tinnitus, headache, nausea, vertigo, disturbed vision). o Notify prescriber is these symptoms develop.
- Monitor the ECG for signs of cardiotoxicity, especially widening of the QRS complex (by 50% or more) and excessive prolongation of the QT interval. o Monitor pulses for significant changes in rate or regularity. If signs of cardiotoxicity develop, withhold quinidine and notify the prescriber.
- Embolism may occur during therapy of atrial fibrillation. o Risk is reduced by treatment with an anticoagulant (e., warfarin, dabigatran). Observe for signs of thromboembolism (e., sudden chest pain, dyspnea), and report these immediately.
- Lidocaine: Acute management of ventricular dysrhythmias.
- Obtain a baseline ECG and determine blood pressure. o Lidocaine is contraindicated for patients with Stokes-Adams syndrome, Wolff-Parkinson-White syndrome, and severe degrees of SA, AV, or intraventricular block in the absence of electronic pacing. o Exercise caution in patients with hepatic dysfunction or impaired hepatic blood flow.
- Mostly IV use, rarely IM for emergencies o Make certain the lidocaine preparation is labeled for IV use (i., is devoid of preservatives and catecholamines).
Dilute concentrated preparations with 5% dextrose in water. o The initial dose is 50 to 100 mg (1 mg/kg) infused at a rate of 25 to 50 mg/min. For maintenance, monitor the ECG and adjust the infusion rate on the basis of cardiac response. The usual rate is 1 to 4 mg/min. o Reserve IM for emergencies. The usual dose is 300 mg injected into the deltoid muscle. Switch to IV lidocaine as soon as possible.
Continuous ECG monitoring is required. o Plasma drug levels should be kept between 1 and 5 mcg/mL.
Excessive doses can cause convulsions and respiratory arrest. o Equipment for resuscitation should be available. o Seizures can be managed with diazepam.
Amiodarone: Long-term treatment of: o atrial fibrillation o life-threatening recurrent ventricular fibrillation or recurrent hemodynamically unstable ventricular tachycardia in patients who have not responded to safer drugs. o (IV use) Initial treatment of recurrent ventricular fibrillation, shock-resistant ventricular fibrillation, recurrent hemodynamically unstable ventricular tachycardia, atrial fibrillation, and AV nodal reentrant tachycardia. o Obtain a baseline ECG, eye examination, and chest x-ray, along with potassium and magnesium levels and tests for thyroid, pulmonary, and liver function. o Amiodarone is contraindicated for patients with severe sinus node dysfunction or second- or third- degree AV block and for women who are pregnant or breastfeeding. o Exercise caution in patients with thyroid disorders, hypokalemia, or hypomagnesemia.
Initiate treatment in a hospital. o High doses are used initially (800 to 1600 mg/day for 1 to 3 weeks). o The usual maintenance dosage is 400 mg/day.
(IV use) Administer by continuous IV infusion, starting with a rapid infusion rate and later reducing the rate for maintenance. o Intravenous treatment may last from 2 days to 3 weeks.
Monitor for beneficial changes in the ECG.
Amiodarone can cause potentially fatal lung damage (hypersensitivity pneumonitis, interstitial/alveolar pneumonitis, and pulmonary fibrosis). o Obtain a baseline chest x-ray and pulmonary function test, and monitor pulmonary function throughout treatment. o Inform patients about signs of lung injury (dyspnea, cough, chest pain), and instruct them to report these immediately. Treatment consists of withdrawing amiodarone and providing supportive care, sometimes including glucocorticoids.
Amiodarone can cause HF and atrial and ventricular dysrhythmias. o Patients with pre-existing heart failure must not use the drug. o Warn patients about signs of HF (e., shortness of breath, reduced exercise tolerance, fatigue, tachycardia, weight gain), and instruct them to report these immediately.
Amiodarone can injure the liver. o Obtain tests of liver function at baseline and periodically during treatment. If circulating liver enzymes exceed 3 times the normal level, amiodarone should be withdrawn.
Adverse Effects: Statins are generally well tolerated. Side effects are uncommon. o Some patients develop headache, rash, memory loss, or GI disturbances (dyspepsia, cramps, flatulence, constipation, abdominal pain).
Statins can injure muscle tissue o Characteristic symptoms are muscles aches, tenderness, or weakness that may be diffuse or localized to certain muscle groups. o Rarely, mild injury progresses to myositis injured muscle. Release of potassium from muscle may cause blood potassium concentrations to rise. o Rarely, myositis progresses to potentially fatal rhabdomyolysis, defined as muscle disintegration or dissolution. Release of muscle components leads to marked elevations of blood CK (greater than 10 times the upper limit of normal [ULN]) and elevations of free myoglobin. o High levels of CK, in turn, may cause renal impairment, as excess CK can plug up the glomeruli, thereby preventing normal filtration.
Fortunately, fatal rhabdomyolysis is extremely rare o Nonetheless, patients should be informed about the risk of myopathy and instructed to notify the prescriber if unexplained muscle pain or tenderness occurs. How statins cause myopathy is unknown.
Liver injury, as evidenced by elevations in serum transaminase levels, develops in 0% to 2% of patients treated 1 year or longer. o However, jaundice and other clinical signs are rare. o Progression to outright liver failure occurs very rarely. o Because of the risk of liver injury, product labeling recommends that liver function tests (LFTs) be done before treatment and then if clinically indicated after starting the drug. If serum transaminase levels rise to 3 times the ULN and remain there, statins should be discontinued. Transaminase levels decline to pretreatment levels following drug withdrawal.
The risk of developing new-onset diabetes while taking a statin is 1 in 500 patients prescribed a statin. o It is unclear whether taking a statin accelerates the advancement from prediabetes to diabetes. Despite the possibility, the CV benefits of taking a statin far outweigh the risk, and management should not change.
Some patients have reported reversible memory loss or confusion that improves after stopping statin therapy.
May cause cataracts. o The greatest risk appears to be in patients taking simvastatin, lovastatin, and atorvastatin. Overall, the risk remains small, and statin therapy should be continued in patients when indicated.
Drug interactions: Combining a statin with most other lipid-lowering drugs (except probably the bile-acid sequestrants) can increase the incidence and severity of the most serious statin-related adverse events: muscle injury, liver injury, and kidney damage. o The increase in risk occurs primarily with fibrates (gemfibrozil, fenofibrate), which are commonly combined with statins. The bottom line: When statins are combined with other lipid-lowering agents, use extra caution and monitor for adverse effects more frequently.
Drugs that inhibit CYP3A4 can raise levels of lovastatin and simvastatin substantially and can raise levels of atorvastatin moderately, by slowing their inactivation. o Important inhibitors of CYP3A4 include macrolide antibiotics (e., erythromycin), azole antifungal drugs (e., ketoconazole, itraconazole), HIV protease inhibitors (e., ritonavir), amiodarone (an antidysrhythmic drug), and cyclosporine (an immunosuppressant).
o If these drugs are combined with a statin, increased caution is advised. Some authorities recommend an automatic reduction in statin dosage if these inhibitors are used.
- Furthermore, the inhibition may persist for 3 days or more after eating the fruit or drinking its juice. o Accordingly, statin users should avoid grapefruits and their juice.
- Cautions: In patients with hepatic impairment, bioavailability of ezetimibe is significantly increased. o At this time, it is not known if increased availability is harmful. Until more is known, patients with moderate or severe hepatic insufficiency should not be given the drug.
- Nursing Care for Antianginal Agents: Therapeutic Goal/ Use/ Technique of Administration
- Nitroglycerin: Reduction of the frequency and intensity of anginal attacks
- (oral Tablets) Instruct patients to place the tablet or empty the powder under the tongue, while in lying or sitting position, and leave it there until fully dissolved; these medications should not be swallowed. o Instruct patients to call 911 or go to an emergency department if pain is not relieved in 5 minutes. While awaiting emergency care, they can take 1 more dose and then a third 5 minutes later.
- Instruct patients to store tablets in a dry place at room temperature in their original container to protect from heat and light, which should be closed tightly after each use. o Under these conditions, the tablets should remain effective until the expiration date on the container.
- (sustained release tablets) Sustained protection against anginal attacks. o To avoid tolerance, administer only once or twice daily. o Instruct patients to swallow these preparations intact, without chewing or crushing.
- (transdermal delivery) Sustained protection against anginal attacks. o Instruct patients to apply transdermal patches to a hairless area of skin, using a new patch and a different site each day. o Instruct patients to remove the patch after 12 to 14 hours, allowing 10 to 12 “patch-free” hours each day. This will prevent tolerance.
- (translingual spray) Prophylaxis or termination of an acute anginal attack. o Instruct patients to direct the spray against the oral mucosa. Warn patients not to inhale the spray.
- (Topical Ointment) Sustained protection against anginal attacks. Instruct patients to remove any remaining ointment before applying a new dose. o Squeeze a ribbon of ointment of prescribed length onto the applicator paper provided o using the applicator paper, spread the ointment over an area at least 2 inches by 3 inches (application may be made to the chest, back, abdomen, upper arm, or anterior thigh) o cover the ointment with plastic wrap. Avoid touching the ointment. Instruct patients to rotate the application site to minimize local irritation.
- (IV use) Angina pectoris refractory to more conventional therapy o perioperative control of blood pressure o production of controlled hypotension during surgery o heart failure associated with acute MI
- Infuse IV using a glass IV bottle and the administration set provided by the manufacturer; avoid standard IV tubing. o Check the stock solution label to verify volume and concentration, which can differ among manufacturers. o Dilute stock solutions before use. o Administer by continuous infusion.
o Because of these advantages, LMW heparins are now considered first-line therapy for prevention and treatment of DVT. Two LMW heparins are available: enoxaparin [Lovenox] and dalteparin [Fragmin].
- LMW heparins are approved for: o prevention of DVT following abdominal surgery, hip replacement surgery, or knee replacement surgery o treatment of established DVT, with or without PE o prevention of ischemic complications in patients with unstable angina, non–Q-wave MI, and ST- elevation MI (STEMI). o In addition, these drugs have been used extensively off label to prevent DVT after general surgery and in patients with multiple trauma and acute spinal injury.
- All LMW heparins are administered subQ. o Dosage is sometimes based on body weight, depending on indication. o Because LMW heparins have an extended half-life, dosing can be done once or twice daily. For prophylaxis of DVT, dosing is begun in the perioperative period and continued 5 to 10 days.
- Dabigatran: is an oral prodrug that undergoes rapid conversion to dabigatran, a reversible, direct thrombin inhibitor o dabigatran has five major advantages: rapid onset; no need to monitor anticoagulation; few drug- food interactions; lower risk of major bleeding; and, since responses are predictable, the same dose can be used for all patients, regardless of age or weight.
- In the United States, dabigatran is approved for the treatment of DVT and PE, as well as for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. o Dabigatran is approved for prevention of VTE following knee or hip replacement surgery. o In 2014, the FDA approved dabigatran for the treatment of DVT and PE in patients who have been treated with a parenteral anticoagulant for 5 to 10 days, and to reduce the risk of recurrent DVT and PE in patients who have been previously treated.
- Dabigatran etexilate [Pradaxa] is available in three strengths: 75-, 110-, and 150-mg capsules. o Dosing may be done with or without food. Patients should swallow the capsules intact. o If the capsules are crushed, chewed, or opened, absorption will be increased by 75%, thereby posing a risk of bleeding.
- The usual dosage for atrial fibrillation is 150 mg twice daily. o If a dose is missed, it should be taken as soon as possible on the same day. However, if the missed dose cannot be taken at least 6 hours before the next scheduled dose, the missed dose should be skipped.
- In patients with significant renal impairment (CrCl 15 to 30 mL/min), the dosage is 75 mg twice a day. o For patients with greater renal impairment (CrCl below 15 mL/min), no dosing recommendation can be made.
- Discontinue warfarin, wait until the INR falls below 2, and then start dabigatran.
- Anticoagulant Nursing Considerations: Administration/ Evaluating Treatment/ Minimizing Adverse Effects/ Minimizing Adverse Interactions
- Heparin: Intravenous (continuous infusion or intermittent) and subQ. Avoid IM injections! o Dosage is prescribed in units, not milligrams. o Heparin preparations vary widely in concentration; read the label carefully to ensure correct dosing. o Administer continuous IV infusion with a continuous infusion pump or some other approved volume- control unit.
Policy may require that dosage be double-checked by a second person. Check the infusion rate every 30 to 60 minutes. During the early phase of treatment, the aPTT or anti-Xa level should be determined every 6 hours.
- Treatment is evaluated by measuring the aPTT or the anti-Xa level. Heparin should increase the aPTT by 1- to 2-fold above baseline. o Therapeutic range for anti-Xa level is 0 to 0 IU/mL.
- Heparin overdose may cause hemorrhage. o Symptoms include reduced blood pressure, elevated heart rate, discolored urine or stool, bruises, petechiae, hematomas, persistent headache or faintness (suggestive of cerebral hemorrhage), pelvic pain (suggestive of ovarian hemorrhage), and lumbar pain (suggestive of adrenal hemorrhage). o Laboratory data suggesting hemorrhage include reductions in the hematocrit and blood cell counts o Severe overdose can be treated with protamine sulfate administered by slow IV injection. The risk of bleeding can be reduced by ensuring that the aPTT or the anti-Xa levels are not above recommended range according to facility protocol.
- HIT, characterized by reduced platelet counts and increased thrombotic events, poses a risk of DVT, PE, cerebral thrombosis, MI, and ischemic injury to the arms and legs. o To reduce risk, monitor platelet counts 2 to 3 times a week during the first 3 weeks of heparin use, and monthly thereafter. If severe thrombocytopenia develops (platelet count below 100,000/mm3), discontinue heparin and, if anticoagulation is still needed, substitute another anticoagulant, such as argatroban.
- Heparin and all other anticoagulants pose a risk of spinal or epidural hematoma in patients undergoing spinal puncture or spinal/epidural anesthesia. o Prolonged or permanent paralysis can result. o Risk of hematoma is increased by several factors, including use of an indwelling epidural catheter, use of other anticoagulants (e., warfarin, dabigatran), and use of antiplatelet drugs (e., aspirin, clopidogrel). Monitor for signs and symptoms of neurologic impairment. If impairment develops, immediate intervention is needed.
- Allergy may develop to antigens in heparin preparations. o To minimize the risk of severe reactions, administer a small test dose before the full therapeutic dose.
- Concurrent use of aspirin, clopidogrel, and other antiplatelet drugs increases the risk of bleeding. Thrombolytic Drugs: Description and Mechanism/ Therapeutic Uses
- Warfarin: The goal is to prevent thrombosis without inducing spontaneous bleeding. o Specific indications include prevention of venous thrombosis and associated PE, prevention of thromboembolism in patients with prosthetic heart valves, and prevention of stroke and systemic embolism in patients with atrial fibrillation.
- For most patients, dosage is adjusted to maintain an INR value of 2 to 3.
- Evaluate therapy by monitoring PT. o The INR should be determined frequently: daily during the first 5 days, twice a week for the next 1 to 2 weeks, once a week for the next 1 to 2 months, and every 2 to 4 weeks thereafter. o In addition, the INR should be determined whenever a drug that interacts with warfarin is added to or withdrawn from the regimen. o When appropriate, teach patients how to monitor their PT and INR at home.
- Hemorrhage is the major complication of warfarin therapy. o Instruct the patient to withhold warfarin and notify the prescriber if signs of bleeding are noted.
o thrombolysis develops faster, and emergency personnel are spared the trouble of monitoring a prolonged infusion. Because tenecteplase is so easy to administer, it has the potential to allow dosing before the patient reaches a hospital. 13. Myocardial Infarction Agents: Management of STEMI/ Oxygen/ Aspirin/ NSAIDS/ Morphine/ Beta- Blockers/ Nitroglycerin
- When a patient presents with suspected STEMI, several interventions should begin immediately. o The objective is to minimize possible myocardial necrosis while waiting for a clear diagnosis. o Once STEMI has been diagnosed, more definitive therapy—reperfusion—can be implemented
- Supplemental oxygen, administered by nasal cannula, can increase arterial oxygen saturation and can thereby increase oxygen delivery to the ischemic myocardium.
- Accordingly, current guidelines recommend giving oxygen to all patients with reduced arterial oxygen saturation (below 90%). o However, although oxygen is recommended and using it seems to make sense, the practice is not evidence based. That is, we have no hard evidence to show that oxygen is beneficial. In fact, there is some evidence that oxygen may actually be harmful, causing mortality to increase rather than decline.
- Aspirin suppresses platelet aggregation, producing an immediate antithrombotic effect o all patients with evolving STEMI should get aspirin. o Therapy should begin immediately after onset of symptoms and should continue indefinitely. o The first dose (162 to 325 mg) should be chewed to allow rapid absorption across the buccal mucosa. Prolonged therapy (with 81 to 162 mg/day) reduces the risk of reinfarction, stroke, and death.
- Routine use of nonsteroidal anti-inflammatory drugs (NSAIDs) other than aspirin should be discontinued. o these agents increase the risk of mortality, reinfarction, hypertension, heart failure, and myocardial rupture.
- Intravenous morphine is the treatment of choice for STEMI-associated pain. o By promoting venodilation, the drug reduces cardiac preload. o By promoting modest arterial dilation, morphine may cause some reduction in afterload. The combined reductions in preload and afterload lower cardiac oxygen demand, helping preserve the ischemic myocardium.
- When given to patients undergoing acute STEMI, beta blockers (e., atenolol, metoprolol) reduce cardiac pain, infarct size, and short-term mortality. o Recurrent ischemia and reinfarction are also decreased. o Reduction in myocardial wall tension may decrease the risk of myocardial rupture.
- As STEMI evolves, traffic along sympathetic nerves to the heart increases greatly, as does the number of beta receptors in the heart. o As a result, heart rate and force of contraction rise substantially, increasing cardiac oxygen demand. o By preventing beta-receptor activation, beta blockers reduce heart rate and contractility, and thereby reduce oxygen demand. o They reduce oxygen demand even more by lowering blood pressure. o By prolonging diastolic filling time, beta blockers increase coronary blood flow and myocardial oxygen supply. Additional benefits derive from antidysrhythmic actions.
o good for patients with reflex tachycardia, systolic hypertension, atrial fibrillation, and atrioventricular conduction abnormalities. Contraindications include overt severe heart failure, pronounced bradycardia, persistent hypotension, advanced heart block, and cardiogenic shock.
- In patients with STEMI, nitroglycerin has several beneficial effects: o reduce preload and thereby reduce oxygen demand o increase collateral blood flow in the ischemic region of the heart o control hypertension caused by STEMI-associated anxiety o limit infarct size and improve LV function. However, despite these useful effects, nitroglycerin does not reduce mortality o Indications for IV therapy include persisting ischemic discomfort, hypertension, and pulmonary congestion. Nitroglycerin should be avoided in patients with hypotension (systolic pressure below 90 mm Hg), severe bradycardia (heart rate below 50 beats/min), marked tachycardia (heart rate above 100 beats/min) or suspected right ventricular infarction. In addition, nitroglycerin should be avoided in patients who have taken sildenafil, avanafil, or vardenafil for erectile dysfunction or pulmonary hypertension within the past 24 hours or tadalafil within the past 48 hours.
- Nursing Care for Deficiency Anemia Agents: Therapeutic Goal, Baseline Data, Ongoing Evaluation and Interventions
Iron Preparations: Prevention or treatment of iron deficiency anemias.
Before treatment, assess the degree of anemia. o Fatigue, listlessness, and pallor indicate mild anemia; dyspnea, tachycardia, and angina suggest severe anemia. o Laboratory findings indicative of anemia are subnormal hemoglobin levels, subnormal hematocrit, subnormal hemosiderin in bone marrow, and the presence of microcytic, hypochromic erythrocytes. The cause of iron deficiency (e., pregnancy, occult bleeding, menorrhagia, inadequate diet, malabsorption) must be determined.
If the diet is low in iron, advise the patient to increase consumption of iron-rich foods (e., egg yolks, brewer's yeast, wheat germ, muscle meats, fish, fowl).
Evaluate treatment by monitoring hematologic status. o Reticulocyte counts should increase within 4 to 7 days, hemoglobin content and the hematocrit should begin to rise within 1 week, and hemoglobin levels should rise by at least 2 gm/dL within 1 month. If these responses do not occur, evaluate the patient for adherence, persistent bleeding, inflammatory disease, and malabsorption.
Forewarn patients about possible GI reactions (nausea, vomiting, constipation, diarrhea) and inform them these will diminish over time. o If GI distress is severe, the dosage may be reduced, or if absolutely necessary, iron may be administered with food.
Inform patients that iron will impart a harmless dark green or black color to stools.
Parenteral iron dextran (and, rarely, SFGC, iron sucrose, and ferumoxytol) can cause potentially fatal anaphylaxis. o Before giving parenteral iron, ensure that injectable epinephrine and facilities for resuscitation are immediately available. o After administration, observe the patient for 60 minutes. Give test doses as described earlier.
Monitor hematologic status. o Within 2 weeks, megaloblasts should disappear, reticulocyte counts should increase, and the hematocrit should begin to rise. Module 11 & 12
- Depression Agents: Fluoxetine, Mechanism of Action/ Therapeutic Uses/ Adverse Effects, Venlafaxine, Duloxetine
- Fluoxetine: As shown, SSRIs selectively block neuronal reuptake of serotonin (5-hydroxytryptamine [5-HT]), a monoamine neurotransmitter. o As a result of reuptake blockade, the concentration of 5-HT in the synapse increases, causing increased activation of postsynaptic 5-HT receptors. o therapeutic effects are the result of adaptive cellular changes that take place in response to prolonged reuptake blockade. o Fluoxetine and the other SSRIs do not block reuptake of dopamine or norepinephrine (NE). o fluoxetine produces CNS excitation rather than sedation.
- Fluoxetine is used primarily for major depression. o In addition, the drug is approved for bipolar disorder, obsessive-compulsive disorder, panic disorder, bulimia nervosa, and premenstrual dysphoric disorder. o Unlabeled uses include post-traumatic stress disorder, social phobia, alcoholism, attention-deficit/hyperactivity disorder, migraine, and Tourette's syndrome.
- Fluoxetine causes sexual problems (impotence, delayed or absent orgasm, delayed or absent ejaculation, decreased sexual interest) in nearly 70% of men and women. o Patients should be informed about the high probability of sexual dysfunction and told to report any problems so that they can be addressed.
- Like many other antidepressants, fluoxetine and other SSRIs cause weight gain. o Although the reason is unknown, a good possibility is decreased sensitivity of 5-HT receptors that regulate appetite.
- By increasing serotonergic transmission in the brainstem and spinal cord, fluoxetine and other SSRIs can cause serotonin syndrome. o This syndrome usually begins 2 to 72 hours after treatment onset. Signs and symptoms include altered mental status (agitation, confusion, disorientation, anxiety, hallucinations, poor concentration) as well as incoordination, myoclonus, hyperreflexia, excessive sweating, tremor, and fever.
- Abrupt discontinuation of SSRIs can cause a withdrawal syndrome. o Symptoms include dizziness, headache, nausea, sensory disturbances, tremor, anxiety, and dysphoria. o it is important to distinguish between symptoms of withdrawal and return of depression.
- Use of fluoxetine and other SSRIs late in pregnancy poses a small risk of two adverse effects in the newborn: o neonatal abstinence syndrome (NAS) o persistent pulmonary hypertension of the newborn (PPHN). o NAS is characterized by irritability, abnormal crying, tremor, respiratory distress, and possibly seizures.
- SSRIs—paroxetine and fluoxetine—may cause septal heart defects. o But even with these agents, the absolute risk is very low.
- SSRIs cause extrapyramidal symptoms (EPS) in about 0% of patients. o the most common EPS is akathisia, characterized by restlessness and agitation.
- SSRIs may cause bruxism (clenching and grinding of teeth).
o Sequelae of bruxism include headache, jaw pain, and dental problems (e., cracked fillings).
- Fluoxetine and other SSRIs can increase the risk of bleeding in the GI tract and at other sites by impeding platelet aggregation. o Platelets require 5-HT for aggregation, but cannot make it themselves and, hence, must take 5-HT up from the blood; by blocking 5-HT uptake, SSRIs suppress aggregation.
- Fluoxetine and other SSRIs have been associated with an increased risk of hemorrhagic stroke. However, a causal relationship has not been established.
- Fluoxetine can cause hyponatremia (serum sodium below 135 mEq/L), probably by increasing secretion of antidiuretic hormone. o Most cases involve older adult patients taking thiazide diuretics
- Fluoxetine may cause dizziness and fatigue; patients who experience intense dizziness and fatigue should be warned against driving and other hazardous activities.
- Skin rash, which can be severe, has occurred in 4% of patients; in most cases, rashes readily respond to drug therapy (antihistamines, glucocorticoids) or to withdrawal of fluoxetine.
- Other common reactions include diarrhea and excessive sweating.
- Venlafaxine: the first SNRI available, is approved for major depression, generalized anxiety disorder, social anxiety disorder (social phobia), and panic disorder.
- The drug produces a powerful blockade of NE and 5-HT reuptake and a weak blockade of dopamine reuptake. o Venlafaxine does not block cholinergic, histaminergic, or alpha 1 -adrenergic receptors.
- Venlafaxine can cause a variety of adverse effects. The most common is nausea followed by headache, anorexia, nervousness, sweating, somnolence, and insomnia.
- Dose-dependent weight loss may occur secondary to anorexia.
- Venlafaxine can also cause dose-related sustained diastolic hypertension; blood pressure should be monitored.
- Sexual dysfunction (e., impotence, anorgasmia) may occur too.
- Some patients experience sustained mydriasis (dilation of the pupil), which can increase the risk of eye injury in those with elevated intraocular pressure or glaucoma.
- Like the SSRIs, venlafaxine can cause hyponatremia, especially in older adult patients taking diuretics.
- Like all other antidepressants, venlafaxine may increase the risk of suicide, especially in children and young adults.
- Combined use of venlafaxine with MAOIs and other serotonergic drugs increases the risk of serotonin syndrome, a potentially fatal reaction o However, combined use with an MAOI is contraindicated. o Accordingly, MAOIs should be withdrawn at least 14 days before starting venlafaxine. o When switching from venlafaxine to an MAOI, venlafaxine should be discontinued 7 days before starting the MAOI.
- As with the SSRIs, use of venlafaxine late in pregnancy can result in a neonatal withdrawal syndrome, characterized by irritability, abnormal crying, tremor, respiratory distress, and possibly seizures. o Symptoms, which can be managed with supportive care, generally abate within a few days.
- Abrupt discontinuation can cause an intense withdrawal syndrome.
- Symptoms include anxiety, agitation, tremors, headache, vertigo, nausea, tachycardia, and tinnitus. o Worsening of pretreatment symptoms may also occur. o Withdrawal symptoms can be minimized by tapering the dosage over 2 to 4 weeks. Warn patients not to stop venlafaxine abruptly.
- Duloxetine: Duloxetine [Cymbalta] was the second SNRI approved for major depression.
- The drug is a powerful inhibitor of 5-HT and NE reuptake, and a much weaker inhibitor of dopamine reuptake.
EXAM 3 Study Guide Pharmacology
Course: Pharmacology (NSG 124)
University: Herzing University

- Discover more from: