- Information
- AI Chat
Pharm 3 - Blueprint
Pharmacology (NSG 124)
Herzing University
Recommended for you
Related Studylists
PharmPreview text
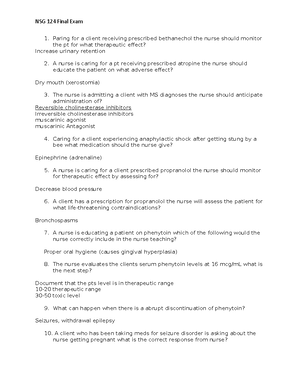
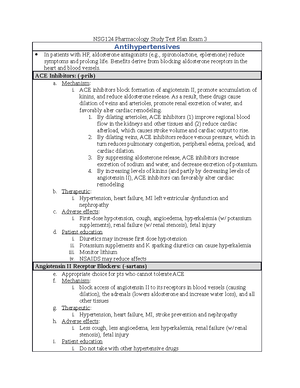
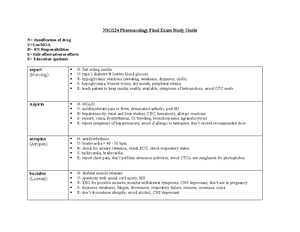
NSG124 Pharmacology Study Test Plan Exam 3
Antihypertensives
In patients with HF, aldosterone antagonists (e., spironolactone, eplerenone) reduce symptoms and prolong life. Benefits derive from blocking aldosterone receptors in the heart and blood vessels. ACE Inhibitors: (-prils) a. Mechanism: i. ACE inhibitors block formation of angiotensin II, promote accumulation of kinins, and reduce aldosterone release. As a result, these drugs cause dilation of veins and arterioles, promote renal excretion of water, and favorably alter cardiac remodeling. 1. By dilating arterioles, ACE inhibitors (1) improve regional blood flow in the kidneys and other tissues and (2) reduce cardiac afterload, which causes stroke volume and cardiac output to rise. 2. By dilating veins, ACE inhibitors reduce venous pressure, which in turn reduces pulmonary congestion, peripheral edema, preload, and cardiac dilation. 3. By suppressing aldosterone release, ACE inhibitors increase excretion of sodium and water, and decrease excretion of potassium. 4. By increasing levels of kinins (and partly by decreasing levels of angiotensin II), ACE inhibitors can favorably alter cardiac remodeling b. Therapeutic: i. Hypertension, heart failure, MI left ventricular dysfunction and nephropathy c. Adverse effects: i. First-dose hypotension, cough, angioedema, hyperkalemia (w/ potassium supplements), renal failure (w/ renal stenosis), fetal injury d. Patient education i. Diuretics may increase first dose hypotension ii. Potassium supplements and K sparking diuretics can cause hyperkalemia iii. Monitor lithium iv. NSAIDS may reduce affects
Angiotensin II Receptor Blockers: (-sartans) e. Appropriate choice for pts who cannot tolerate ACE f. Mechanism: i. block access of angiotensin II to its receptors in blood vessels (causing dilation), the adrenals (lowers aldosterone and increase water loss), and all other tissues g. Therapeutic: i. Hypertension, heart failure, MI, stroke prevention and nephropathy h. Adverse effects: i. Less cough, less angioedema, less hyperkalemia, renal failure (w/ renal stenosis), fetal injury i. Patient education i. Do not take with other hypertensive drugs
ARBs share the beneficial hemodynamic effects of ACE inhibitors, but not the beneficial effects on cardiac remodeling. a. In patients with HF, ARBs should be reserved for patients intolerant of ACE inhibitors (usually owing to cough). Aldosterone antagonists: (eplerenone and spironolactone)
b. Mechanism: i. block receptors for aldosterone c. Therapeutic: i. hypertension and heart failure Patient education o avoid potassium supplements and potassium-containing salt substitutes unless they are prescribed by the provider. Potassium-sparing diuretics must also be avoided. Signs of high potassium – 3.5-5 – muscle spasm o possibility of persistent dry, irritating, nonproductive cough with ACEs and ARBs o do not use during pregnancy o seek immediate medical attention if angioedema develops o neutropenia: early signs of infection (fever, sore throat, mouth sores) o minimize NSAID use Nursing interventions o Stop diuretics o avoiding potassium supplements and potassium-sparing diuretics except when they are clearly indicated o Monitor lithium levels frequently Nursing considerations o ACEs and ARBs taken without regard to meal o Aliskiren should be taken same time each day at mealtime
Calcium Channel Blockers – Verapamil and Nifedipine nifedipine and the other dihydropyridines act primarily on vascular smooth muscle verapamil and diltiazem act on vascular smooth muscle and on the heart Verapamil: o Mechanism: vasodilation accompanied by reduced arterial pressure and increased coronary perfusion o Therapeutic: angina (for vasodilation), hypertension (by dilating arterioles), cardiac dysrhythmias (suppressing impulse conduction through the AV node) o Adverse effects: constipation from blockade calcium channels in smooth muscle of intestine, dizziness, facial flushing, headache, and edema of the ankles and feet from vasodilation can cause bradycardia, partial or complete AV block gingival hyperplasia o Patient education No grapefruit juice Inform patients about signs of edema (swelling in ankles or feet), and instruct them to notify the prescriber if these occur Advise patients that constipation can be minimized by increasing dietary
Vasodilator Agents: drugs that dilate resistance vessels (arterioles) cause a decrease in cardiac afterload (the force the heart works against to pump blood) drugs that dilate capacitance vessels (veins) reduce the force with which blood is returned to the heart, which reduces ventricular filling and decreases cardiac preload (the degree of stretch of the ventricular muscle before contraction), which decreases the force of ventricular contraction Therapeutic uses a. hypertension, hypertensive crisis, angina pectoris, heart failure, and myocardial infarction, pheochromocytoma, peripheral vascular disease, pulmonary arterial hypertension, and production of controlled hypotension during surgery Adverse effects a. Orthostatic hypotension falls, reflex tachycardia, expansion of blood volume, Examples a. Sodium nitroprusside: i. acts faster than any other vasodilator available / drug of choice for hypertensive emergencies and controlled hypotension during surgery / effects begin in seconds and then fade rapidly when administration ceases ii. direct-acting vasodilator that relaxes smooth muscle of arterioles and veins iii. IV infusion, can trigger retention of sodium and water; furosemide can help counteract this effect iv. Adverse: excessive hypotension, cyanide poisoning from breakdown, thiocyanate accumulation and toxicity v. To avoid hypotension, continuous BP monitoring is required. b. Hydralazine: i. Causes selective dilation of arterioles ii. Can cause syndrome that resembles SLE c. Minoxidil: i. causes selective and profound dilation of arterioles ii. can cause hypertrichosis
Diuretics are first-line drugs for all patients with fluid overload. By reducing blood volume, these drugs can decrease venous pressure, arterial pressure, pulmonary edema, peripheral edema, and cardiac dilation - do not prolong survival o Thiazide diuretics are ineffective when GFR is low, and cannot be used if cardiac output is greatly reduced. o Loop diuretics are effective even when GFR is low, and are preferred to thiazides for most patients. o Thiazide diuretics and loop diuretics can cause hypokalemia and can increase the risk of digoxin-induced dysrhythmias
o Potassium-sparing diuretics are used to counteract potassium loss caused by thiazide diuretics and loop diuretics o Potassium-sparing diuretics can cause hyperkalemia. By doing so, they can increase the risk of hyperkalemia in patients taking ACE inhibitors or ARBs
Beta blockers BB can prolong survival in patients with HF and are considered first-line therapy To avoid excessive cardiosuppression, beta-blocker dosage must be very low initially and then gradually increased. Isosorbide dinitrate (which dilates veins) plus hydralazine (which dilates arterioles) can be used in place of an ACE inhibitor (or ARB) if an ACE inhibitor (or ARB) cannot be used. BiDil, a fixed-dose combination of hydralazine and isosorbide dinitrate, is approved specifically for treating HF in African Americans.
Digoxin Digoxin and other inotropic agents increase the force of myocardial contraction and thereby increase cardiac output. Of the available inotropic agents, digoxin is the only one that is both effective and safe when used orally and the only one suitable for long-term use. Digoxin increases contractility by inhibiting myocardial Na+/K+-ATPase, thereby (indirectly) increasing intracellular calcium, which in turn facilitates the interaction of actin and myosin. Potassium competes with digoxin for binding to Na+/K+-ATPase. Therefore, if potassium levels are low, excessive inhibition of Na+/K+-ATPase can occur, resulting in toxicity. Conversely, if potassium levels are high, insufficient inhibition can occur, resulting in therapeutic failure. Accordingly, it is imperative to keep potassium levels in the normal physiologic range: 3 to 5 mEq/L. By increasing cardiac output, digoxin can reverse all of the overt manifestations of HF: cardiac output improves, heart rate decreases, heart size declines, constriction of arterioles and veins decreases, water retention reverses, blood volume declines, peripheral and pulmonary edema decrease, water weight is lost, and exercise tolerance improves. Unfortunately, although digoxin can improve symptoms, it does not prolong life. In patients with HF, benefits of digoxin are not due solely to improved cardiac output; neurohormonal effects are important too. Digoxin causes dysrhythmias by altering the electrical properties of the heart (secondary to inhibition of Na+/K+-ATPase). The most common reason for digoxin-related dysrhythmias is diuretic-induced hypokalemia. If a severe digoxin overdose is responsible for dysrhythmias, digoxin levels can be lowered using Fab antibody fragments [Digifab] In addition to dysrhythmias, digoxin can cause GI effects (anorexia, nausea, vomiting) and CNS effects (fatigue, visual disturbances). Gastrointestinal and CNS effects often precede dysrhythmias and therefore can provide advance warning of serious toxicity. Digoxin has a narrow therapeutic range. Digoxin is eliminated by renal excretion.
kidneys with a diuretic, and the RAAS with an ACE inhibitor, ARB, DRI, or aldosterone antagonist. o tailor the regimen to the sensitivities of the patient o encourage them to report objectionable responses o Avoid drugs that can exacerbate comorbid conditions Adverse effects Interactions with oral contraceptives, nonsteroidal anti-inflammatory drugs, glucocorticoids, appetite suppressants, tricyclic antidepressants, monoamine oxidase inhibitors, cyclosporine, erythropoietin, alcohol (in large quantities), and nasal decongestants and other cold remedies.
Antidysrhythmics
Treat only if there is a clear benefit—and then only if the benefit outweighs the risks Class I: Sodium channel blockers
Quinidine: 1A Mechanism: o blocks sodium channels, quinidine slows impulse conduction in the atria, ventricles, and His-Purkinje system. o delays repolarization at these sites, apparently by blocking potassium channels. o Both actions contribute to suppression of dysrhythmias
Nursing considerations o cardiotoxicity, monitor pulses o Quinidine causes diarrhea and other GI symptoms in 33% of patients. These effects frequently force drug withdrawal. o risk of embolism, risk treated with anticoagulant / Observe for signs of thromboembolism (e., sudden chest pain, dyspnea) o antidysrhythmic drugs can exacerbate existing dysrhythmias and generate new ones Nursing interventions o Quinidine can double digoxin levels. When these drugs are combined, digoxin dosage should be reduced. Monitor patients for digoxin toxicity Patient education o take quinidine with meals to avoid diarrhea o inform about symptoms of cinchoism Therapeutic effects o Treatment offers two potential benefits: reduction of symptoms and reduction of mortality. o restoration of a regular pulse rate or a pulse rate without major irregularities or with improved regularity compared with the irregularity that existed before therapy Lidocaine 1B: Mechanism: o class IB agents accelerate repolarization o class IB agents have little or no effect on the ECG o an intravenous agent, is used only for ventricular dysrhythmias Therapeutic: o ventricular dysrhythmias Adverse: o drowsiness, confusion, and paresthesias o toxic doses may produce seizures and respiratory arrest Nursing: o Lidocaine undergoes rapid inactivation by the liver. As a result, it must be administered by continuous IV infusion.
Class II: Beta Blockers
Propranolol: Mechanism: o blocks both beta1- and beta2-adrenergic receptors. Beta1 blockade affects the heart, and beta2 blockade affects the bronchi – ultimately a result of calcium channel blocking o attenuates sympathetic stimulation of the heart, leading to (1) decreased automaticity of the SA node, (2) decreased velocity of conduction through the AV node, and (3) decreased myocardial contractility Therapeutic:
o Adenosine decreases automaticity in the SA node and greatly slows conduction through the AV node Therapeutic o Drug of choice for termination of paroxysmal SVT, including Wolff-Parkinson- White syndrome Nursing: o Adenosine has a very short half-life (less than 10 seconds) and must be given by IV bolus o Remember to avoid grapefruit juice and monitor for edema with calcium channel blockers and amiodarone.
Atherosclerotic drugs
HMG-CoA Reductase Inhibitors (Statins) o Beneficial actions: reduction of LDL, increase in HDL, reduction of triglyceride level, increased bone formation o Therapeutic: Hypercholesterolemia: most effective drugs for lowering LDL cholesterol Primary and Secondary Prevention of CV Events Post MI therapy: better late than never Diabetes: controlling CV risk factors—especially hypertension and high cholesterol—is as important as controlling high blood glucose o Adverse: headache, rash, memory loss, or GI disturbances (dyspepsia, cramps, flatulence, constipation, abdominal pain) myopathy: can cause muscle injury hepatotoxicity: tatins are contraindicated for patients with viral or alcoholic hepatitis, fatty liver. o Nursing: Low doses decrease LDL cholesterol by about 25%, and larger doses decrease levels by as much as 63%. Reductions are significant within 2 weeks and maximal within 4 to 6 weeks. Other: o Niacin removed from use o Bile acid sequestrant (Colesevelam): reduce LDL cholesterol levels, used as an adjunct / nonabsorbable resin that binds (sequesters) bile acids and other substances in the GI tract and thereby prevents their absorption and promotes their excretion Cholestyramine and colestipol—but not colesevelam—can impair absorption of fat-soluble vitamins (A, D, E, and K). Vitamin supplements may be required. Colesevelam does not reduce vitamin absorption. o Fibric acid derivatives, also known as fibrates, are the most effective drugs we have for lowering TG levels
Anticoagulant Drugs
Heparin
o Administered only by injection, cannot be absorbed orally o Mechanism: suppresses coagulation by helping antithrombin inactivate clotting factors, primarily thrombin and factor Xa o Therapeutic: used in emergencies and pulmonary embolism, massive deep vein thrombosis, open heart surgery and renal dialysis to prevent coagulation on devices of extracorporeal circulation / low doses used to prevent clots following surgery o Adverse: Hemorrhage Spinal/epidural hematoma Heparin induced thrombocytopenia: reduced platelet counts (thrombocytopenia) and a seemingly paradoxical increase in thrombotic events o Nursing: safe during pregnancy binds variably and so needs to be closely monitored CAUTION with aspirin or other anticoagulant drugs – life threatening LMW heparins for use at home – first choice for DVT treatment – also used with angina Warfarin o Mechanism: suppresses coagulation by decreasing production of Vitamin K dependent clotting factors delayed onset, taken orally, longer duration o Therapeutic: o Adverse: o Nursing:
Direct Thrombin Inhibitors o Mechanism: binds with and inhibits thrombin that is free in the blood, as well as thrombin that is bound to clots o Therapeutic: treatment of DVT and PE, as well as for prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation o Adverse: bleeding, safer than warfarin GI upset can occur, can be taken with food o Nursing: Should be stopped before surgery Thrombolytic: thrombolytic drugs are given to remove thrombi that have already formed Alteplase (tPA)
o Mechanism: binds with plasminogen to form an active complex. The alteplase- plasminogen complex then catalyzes the conversion of other plasminogen molecules into plasmin, an enzyme that digests the fibrin meshwork of clots o Therapeutic: (1) acute MI, (2) acute ischemic stroke, and (3) acute massive PE. o Adverse: (1) plasmin can destroy pre-existing clots, promote recurrence of bleeding at sites of recently healed injury, (2) plasmin can disrupt coagulation and can thereby interfere with new clot formation in response to vascular injury Tenecteplase o Approved only for acute MI o Much longer half-life o Much easier to use o 80x stronger?
In patients with acute MI, ACE inhibitors decrease mortality, severe heart failure, and recurrent MI. All patients should receive an ACE inhibitor in the absence of specific contraindications. For patients who cannot tolerate ACE inhibitors, an ARB may be used instead.
To lower the risk of a second MI, all patients should decrease cardiovascular risk factors (e., smoking, hypercholesterolemia, hypertension, diabetes), exercise for 30 minutes at least 3 or 4 days a week, and undergo long-term therapy with four drugs: a beta blocker, an ACE inhibitor or an ARB, an antiplatelet drug or warfarin, and a statin.
Deficiency Anemia Agents
The principal cause of iron deficiency is increased iron demand secondary to (1) maternal and fetal blood volume expansion during pregnancy; (2) blood volume expansion during infancy and early childhood; or (3) chronic blood loss, usually of GI or uterine origin. The major consequence of iron deficiency is microcytic, hypochromic anemia. Ferrous sulfate, given PO, is the drug of choice for iron deficiency. Iron-deficient patients who cannot tolerate or absorb oral ferrous salts are treated with parenteral iron—usually iron dextran administered IV. The major adverse effects of ferrous sulfate are GI disturbances. These are best managed by reducing the dosage (rather than by administering the drug with food, which would greatly reduce absorption). Parenteral iron dextran carries a significant risk of fatal anaphylactic reactions. The risk is much lower with other parenteral iron products (e., iron sucrose). When iron dextran is used, a small test dose is required before each full dose. Be aware, however, that patients can experience anaphylaxis and other hypersensitivity reactions from the test dose, and patients who did not react to the test dose may still have these reactions with the full dose. The principal cause of vitamin B12 deficiency is impaired absorption secondary to lack of intrinsic factor. The principal consequences of B12 deficiency are megaloblastic (macrocytic) anemia and neurologic injury. Vitamin B12 deficiency caused by malabsorption is treated lifelong with cyanocobalamin. Traditional treatment consists of IM injections administered monthly. However, large oral doses administered daily are also effective, as are intranasal doses (administered weekly with Nascobal). For initial therapy of severe vitamin B12 deficiency, parenteral folic acid is given along with cyanocobalamin. When folic acid is combined with vitamin B12 to treat B12 deficiency, it is essential that the dosage of B12 be adequate because folic acid can mask continued B12 deficiency (by improving the hematologic picture), while allowing the neurologic consequences of B deficiency to progress. The principal causes of folic acid deficiency are poor diet (usually in patients with alcohol use disorder) and malabsorption secondary to intestinal disease. The principal consequences of folic acid deficiency are megaloblastic anemia and neural tube defects in the developing fetus. To prevent neural tube defects, all women who may become pregnant should ingest 400 to 800 mcg of supplemental folate daily, in addition to the folate they get in food.
Desvenlafaxine = major metabolite of venlafaxine, only approved for depression Duloxetine = benefits may begin quickly, 2 weeks, also fibromyalgia, generalized anxiety disorder, pain of diabetic peripheral neuropathy, and chronic musculoskeletal pain, including low back pain and pain from osteoarthritis
Bupropion Mechanism o unique antidepressant similar in structure to amphetamine o unclear, but may be related to blockade of dopamine and/or NE reuptake o does not affect serotonergic, cholinergic, or histaminergic transmission, and does not inhibit MAO Therapeutic o (1) major depressive disorder and o (2) prevention of seasonal affective disorder (SAD) o Also smoking cessation, treatment of depression in bipolar, ADHD management Adverse o agitation, headache, dry mouth, constipation, weight loss, GI upset, dizziness, tremor, insomnia, blurred vision, and tachycardia o can cause seizures, psychotic symptoms Nursing o Do not combine with MAOIs, some SSRIs
Mirtazapine
Mechanism o increased release of 5-HT and NE by blocking receptors that inhibit release Therapeutic o antidepressant Adverse o blocks histamine receptors and thus promotes sedation and weight gain Nursing considerations o Tricyclics: Use TCAs with caution in patients with cardiac disorders (e., coronary heart disease, progressive heart failure, paroxysmal tachycardia), elevated intraocular pressure, urinary retention, hyperthyroidism, seizure disorders, and liver or kidney dysfunction. Orthostatic hypotension, diaphoresis and anticholinergic effects with TCAs Cardiotoxicity and hypomania o MAOIs First choice for atypical depression MAOIs are contraindicated for patients taking SSRIs; for patients with pheochromocytoma, heart failure, liver disease, severe renal impairment, cerebrovascular defect Hypertensive crisis with dietary tyramine or sympathomimetics – provide list of what to avoid Orthostatic hypotension
Pharm 3 - Blueprint
Course: Pharmacology (NSG 124)
University: Herzing University

- Discover more from: