- Information
- AI Chat
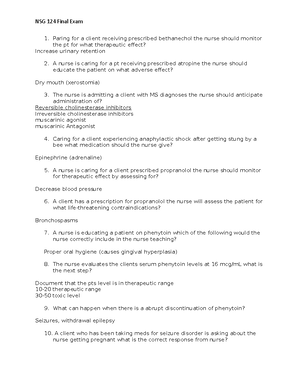
Pharmacology Exam 4 Study Guide
Pharmacology (NSG 124)
Herzing University
Recommended for you
Related Studylists
Pharm (NSG 124)Preview text
gPharmacology Exam 4 Study Guide
Modules 9 and 10 Renin-Angiotensin-Aldosterone Drugs & Nursing Care Angiotensin converting enzyme (ACE) inhibitors End in -pril Therapeutic Uses Hypertension Heart failure Myocardial infarction (MI) Diabetic and nondiabetic nephropathy Prevention of MI, stroke, and death in pts at high cardiovascular risk Adverse effects First dose hypotension More likely to occur in pts with sever hypertension, pts taking diuretics, and pts who are sodium depleted or volume depleted Fetal injury (no ACEs during pregnancy) Cough Angioedema Hyperkalemia Renal failure Inhibition of aldosterone release can cause potassium retention Neutropenia Specific effects include hypotension, hyperkalemia, skull hypoplasia, pulmonary hypoplasia, anuria, renal failure (reversible and irreversible), and death Identifying high-risk patients Drug interactions Diuretics Antihypertensive agents Drugs that raise potassium levels Lithium ACEs can cause lithium to accumulate to toxic levels NSAIDs May reduce the antihypertensive effects of ACEs Minimizing adverse effects Angiotensin II receptor blockers (ARBs) End in -sartan Therapeutic uses Hypertension, heart failure, myocardial infarction Diabetic nephropathy Pt unable to tolerate ACE inhibitors – protection against MI, stroke, and death from CV causes in high risk pts May prevent development of diabetic retinopathy
Not effective for primary prevention of nephropathy in normotensive diabetic pts Adverse effects Angioedema Fetal harm Renal failure ARBs do not promote accumulation of bradykinin in the lung and therefore have a lower instance of cough Direct renin inhibitors Aliskiren (Tekturna) Binds tightly with renin and thereby inhibits the cleavage of angiotensinogen into angiotensin I Can reduce the influence of the entire RAA system Side effects Angioedema, cough, GI effects (dose-dependent diarrhea), hyperkalemia, fetal injury, and death Aldosterone antagonists Eplerenone (Inspra) Therapeutic uses Hypertension Heart failure Adverse effects Hyperkalemia Drug interactions Inhibitors of CYP3A Drugs that raise potassium levels Use with caution when combined with lithium Spironolactone (Aldactone) Potassium sparing diuretic Therapeutic uses Hypertension Heart failure Adverse effects Hyperkalemia Gynecomastia Menstrual irregularities Impotence Hirsutism (excessive hair growth in unexpected areas) Deepening of the voice
Nursing Care for Calcium Channel Blockers Classification Non-dihydropyridines – Verapamil and Diltiazem Dihydropyridines – Nifedipine Sites of action Dihydropyridines act primarily on arterioles
Like verapamil, except for less constipation Dizziness Flushing Headache Edema of ankles and feet Exacerbates bradycardia, sick sinus syndrome, heart failure, second- or third-degree heart block Drug interactions Digoxin Beta-adrenergic blocking agents Nifedipine (Adalat CC, Nifedical, Procardia) About Nifedipine Vasodilation by blocking calcium channels Blocks in vascular smooth muscle Very little blockade of heart calcium channels Cannot be used to treat dysrhythmias Less likely than verapamil to exacerbate pre-existing cardiac disorders Mechanism of action Arteriolar dilation causes a direct decrease in arterial pressure or venous dilation reduces cardiac output, which in turn reduces arterial pressure Baroreceptors in the aortic arch and carotid sinus sense the drop in pressure and relay this information to the vasomotor center of the medulla In an attempt to bring B/P back up, the medulla sends impulses along sympathetic nerves instructing the heart to beat faster Therapeutic uses Angina pectoris Hypertension Investigational basis – to relieve migraine headache and to suppress preterm labor Effects of Nifedipine Reflex tachycardia Increases cardiac oxygen demand Can be combined with a beta blocker for prevention of reflex tachycardia Adverse effects Flushing Dizziness Headache Peripheral edema Gingival hyperplasia Chronic eczematous rash in older pts Immediate release (not sustained)
Has been associated with increased mortality in pts with MI and unstable angina Other rapid-acting calcium channel blockers also associated No cause-and-effect relationship established National heart, lung, and blood institute (NHLBI) recommends that these be used with great caution
Vasodilator Agents Vasodilation Can be produced with a variety of drugs Some act primarily on veins or arterioles, others act on both types of vessels Wide variety of therapeutic applications Overview of therapeutic uses Principal indications Essential hypertension Hypertensive crisis Angina pectoris Heart failure Myocardial infarction Pheochromocytoma Peripheral vascular disease Pulmonary arterial hypertension Production of controlled hypotension during surgery Adverse effects related to vasodilation Postural hypotension Teach pt about symptoms of hypotension and advise them to sit or lie down if these occur Reflex tachycardia Expansion of blood volume Hydralazine Selective dilation of arterioles Postural hypotension minimal Therapeutic uses Essential hypertension Hypertensive crisis Heart failure Adverse effects Reflex tachycardia Increased blood volume Systemic lupus erythematosus-like syndrome Headache, dizziness, weakness, and fatigue Symptoms include muscle pain, joint pain, nephritis, pericarditis, and the presence of antinuclear antibodies Drug interactions Other antihypertensive agents
Aldosterone antagonists Direct renin inhibitors – type 2 diabetes mellitus precautions Individualizing therapy Patients with comorbid conditions Renal disease Diabetes Patients in special populations African Americans Children and adolescents Older adults Drugs for hypertensive emergencies Sodium nitroprusside Fenoldopam Labetalol Diazoxide Clevidipine Drugs for hypertensive disorders of pregnancy Chronic hypertension and pregnancy ACE inhibitors, ARBs, and DRIs are contraindicated during pregnancy Most other antihypertensives can be continued during pregnancy Preeclampsia and eclampsia Hydralazine Magnesium sulfate (anticonvulsant) Minimize adverse effects by tailoring the regimen to the sensitivities of the pt and teach self-monitoring
Drugs for Heart Failure Diuretics Thiazide diuretics High-ceiling (loop) diuretics Potassium-sparing diuretics RAAS inhibitors Angiotensin-converting enzyme inhibitors Hemodynamic benefits Arteriolar dilation Venous dilation Suppression of aldosterone release Impact on cardiac remodeling ACE inhibitors have a favorable impact Angiotensin II receptor blockers Clinical trials have shown that ARBs improve LV ejection fraction, reduce HF symptoms, increase exercise tolerance, decrease hospitalization, enhance quality of life, and reduce mortality Aldosterone antagonists Spironolactone (Aldactone) and eplerenone (Inspra)
Current studies recommend adding an aldosterone antagonist to standard HF therapy in pts with moderately or severe symptoms Direct renin inhibitors Benefits in HF should be equal to those of ACE inhibitors or ARBs Aliskiren (Tekturna) is being tested in HF Not yet approved for HF treatment Beta blockers End in -lol Action With careful control of dosage, it can improve pt’s status Protect from excessive sympathetic stimulation Protect against dysthymias Adverse effects Fluid retention of worsening of HF Fatigue Hypotension Bradycardia or heart block Digoxin and cardiac glycosides Positive inotropic actions (affecting the force or speed of muscle contraction) Increase myocardial contractile force Alter electrical activity of the heart Favorable affect neurohormonal systems Increases cardiac output Second-line agents Digoxin (Lanoxin, Lanoxicaps, Digitek) Adverse effect Can cause severe dysrhythmias Predisposing factors Hypokalemia Elevated digoxin level Narrow therapeutic range Heart disease Diagnosing digoxin-induced dysrhythmias Laboratory data required for diagnosis include digoxin level, serum electrolytes, and an ECG Managing digoxin-induced dysrhythmias Withdraw digoxin Monitor serum potassium Some pts may require an antidysrhythmic drug Pts who develop bradycardia or AV block can be treated with atropine Electronic pacing may be employed Digoxin levels can be lowered using fab antibody fragments (Digifab) Noncardiac adverse effects
Inodilator – increase myocardial contractability and promotes vasodilation Reserved for patients with severe reduction in cardiac output resulting in decreased organ perfusion Arrhythmias, myocardial ischemia Ivabradine (Corlanor) For use in pts with stable, symptomatic heart failure with: LVEF <35% Sinus rhythm Heart rate > 70 bpm Can be used for pts who have a contraindication to beta blocker use Hydralazine Vasodilators Isosorbide dinitrate plus hydralazine Intravenous vasodilators for acute care Nitroglycerin Principal adverse effects Hypotension Resultant reflex tachycardia Sodium nitroprusside (Nitropress) Principal adverse effect Profound hypotension Nesiritide (Natrecor) Principal adverse effect Symptomatic hypotension Management of heart failure Drugs to avoid during management of heart failure Antidysrhythmic agents Calcium channel blockers NSAIDs Device therapy Implanted cardioverter-defibrillators Cardiac resynchronization Exercise training Evaluating treatment Based on symptoms and physical findings
Nursing Care for Antidysrhythmic Agents Classifications Class 1 – sodium channel blockers Quinidine Effects on the heart Blocks sodium channels Slow impulse conduction Delays repolarization Blocks vagal input to the heart
Effects on the ECG Widens the QRS complex Prolongs the QT interval Therapeutic uses Used for supraventricular and ventricular dysrhythmias Adverse effects Diarrhea Cinchonism Cardiotoxicity Arterial embolism Alpha-adrenergic blockade, resulting in hypotension Drug interactions Digoxin Class 2 – beta blockers Only 4 approved for treating dysrhythmias Propranolol Acebutolol Esmolol Sotalol Class 3 – potassium channel blockers Amiodarone (Cordarone, Pacerone) Therapeutic uses For life threatening ventricular fibrillation Recurrent hemodynamically unstable ventricular tachycardia Effects on the heart and ECG Reduced automaticity in the SA node Reduced contractility Reduced conduction velocity QRS widening Prolongation of the PR and QT intervals Adverse effects Protracted half-life Pulmonary toxicity Cardiotoxicity Toxicity in pregnancy and breast feeding Corneal microdeposits Optic neuropathy Class 4 – calcium channel blockers Verapamil (calan, Covera, Verelan) and Diltiazem (Cardizem) Reduces SA node automaticity Delay AV nodal conduction Reduce myocardial contractility Therapeutic uses Slow ventricular rate Terminate SVT caused bu am AV node reentrant circuit
Primarily use to relive symptoms of depression Can also help pts with anxiety disorders Not indicated for uncomplicated bereavement Antidepressant groups Tricyclic antidepressants Selective serotonin reuptake inhibitors (SSRIs) Serotonin/Norepinephrine reuptake inhibitors (SNRIs) Monoamine oxidase inhibitors (MAOIs) Atypical antidepressants Basic considerations Time course of response Symptoms resolve slowly Initial responses develop after 1 to 3 weeks Maximal response may not be seen for 12 weeks Failure when taken 1 month without success Drug selection Antidepressants have nearly equal efficacy Suicide risk with antidepressants May increase suicidal tendencies during early treatment Pts should be observed closely for: Suicidality Worsening mood Changes in behavior Precautions Prescriptions should be written for the smallest number of doses consistent with good patient management Dosing of inpatients should be directly observed
SSRI and SNRI Depression Agents Fluoxetine (Prozac, Sarafem) Mechanism of action Therapeutic uses Most widely prescribed SSRI in the world Bipolar disorder OCD Panic disorder Bulimia nervosa Premenstrual dysphoric disorder Off-label uses – PTSD, social phobia, alcoholism, ADHD, Tourette’s syndrome, and obesity Adverse effects Serotonin syndrome Begins 2 to 72 hours after treatment Altered mental status Incoordination, myoclonus (involuntary muscle jerk), hyperreflexia, excessive sweating, tremor, and fever
Deaths have occurred Syndrome resolves spontaneously after discontinuing the drug Increased risk by concurrent use of MAOIs and other drugs Withdrawal syndrome (occurs with abrupt discontinuation) Neonatal effects when used during pregnancy Neonatal abstinence syndrome (NAS) Persistent pulmonary hypertension of the newborn (PPHN) Teratogenesis Extrapyramidal side effects Acute dyskinesia, dystonic reactions, tardive dyskinesia, Parkinsonism, akinesia, akathisia, and neuroleptic malignant syndrome Bruxism Bleeding disorders Sexual dysfunction Impotence, delayed or absent orgasm, delayed or absent ejaculation, and decreased sexual interest Weight gain Drug interactions Monoamine oxidase inhibitors Risk of serotonin syndrome Antiplatelet drugs and anticoagulants Aspirin and NSAIDs Warfarin TCAs and lithium Can elevate levels of these drugs Venlafaxine (Effexor) Indications Major depression Generalized anxiety disorder Social anxiety disorder Blocks BE and serotonin uptake Serious reactions if combined with MAOIs Side effects Nausea, headache, anorexia, nervousness, sweating, somnolence, insomnia, weight loss, diastolic hypertension, sexual dysfunction, hyponatremia (in older adult pts), neonatal withdrawal syndrome Duloxetine (Cymbalta) Adverse effects Nausea, somnolence, dry mouth, sweating, insomnia, blurred vision Effects in pregnancy and lactation Drug interactions MAOIs Alcohol
Monoamine Oxidase Inhibitors (MAOI) General information Second or third choice antidepressant for most pts As effective as TCAs and SSRIs but more hazardous Risk of triggering hypertensive crisis if pt eats food rich in tyramine Drug of choice for atypical depression Isocarboxazid (Marplan) Phenelzine (Nardil) Tranylcypromine (Parnate) Therapeutic uses Depression Other uses Bulimia nervosa Agoraphobia ADHD OCD Panic attacks Adverse effects CNS stimulation Orthostatic hypotension Hypertensive crisis from dietary tyramine Tyramine – promotes the release of NE from sympathetic neurons Hypertensive crisis Severe headache, tachycardia, hypertension, nausea and vomiting, confusion, profuse sweating, stroke, and death Treatment – intravenous vasodilator Sodium nitroprusside (a nitric oxide donor) Phentolamine (an alpha-adrenergic antagonist) Labetalol (an alpha-adrenergic and beta-adrenergic antagonist) Drug interactions Indirect-acting sympathomimetic agents Interactions secondary to the inhibition of hepatic MAO Antidepressants – TCAs and SSRIs Antihypertensive drugs Meperidine Transdermal MAOI – Selegiline First transdermal treatment for depression Much lower risk of hypertensive crisis with transdermal route as compared with oral route Enters the system without going through the GI tract Adverse effects still occur when used with sympathomimetic drugs Avoid carbamazepine (Tegretol) and oxcarbazepine (Trileptal)
Atypical Antidepressants Bupropion (Wellbutrin)
Actions and uses Acts as a stimulant and suppresses appetite Antidepressant effects being in 1 to 3 weeks Does not affect serotonergic, cholinergic, or histaminergic transmission Does not cause weight gain Less sexual side effects Adverse effects Seizures Agitation Tremor Tachycardia Blurred vision Dizziness Headache Insomnia Dry mouth GI upset Constipation Weight loss Drug interactions MAOIs can increase the risk of bupropion toxicity Other atypical antidepressants Mirtazapine (Remeron) Nefazodone (Serzone) Trazadone (Oleptro_ Vilazodone (VVilbryd) Amoxapine
Antidepressant Agent Nursing Considerations Promoting adherence Minimizing adverse reactions Minimizing adverse effects
Antianxiety Agents General anxiety disorder treatment Buspirone Not a CNS depressant Has no abuse potential Does not intensify the effects of CNS depressants Anxiolytic effects develop slowly Actions and therapeutic uses Benzodiazepines Ativan, Xanax, Valium Adverse effects Dizziness
Clomipramine Less tolerated Second-line drug Social anxiety disorder Characteristics Intense and irrational fear that one will be scrutinized by others Generalized Nongeneralized Very debilitating Treatment Psychotherapy Drug therapy – SSRIs, paroxetine (Paxil), and sertraline (Zoloft) Post-traumatic stress disorder Characteristics Develops after a traumatic event Re-experiencing the event Avoid reminders of the event Persistent state of hyperarousal Treatment Psychotherapy with drugs Evidence of efficacy is strongest for three SSRIs (fluoxetine, paroxetine, and sertraline) and one SNRI (venlafaxine Psychotherapy alone
Bipolar Disorders and Nondrug Therapies Definition of BPD Cyclic disorder Recurrent fluctuations in mood Episodes of mania and depression persist for months without treatment Types of mood episodes seen with BPD Pure manic episode (euphoric mania) Hypomanic episode (hypomania) Major depressive episodes (depression) Mixed episode Treatment Drugs Mood stabilizers – lithium, divalproex sodium, and carbamazepine Relieves symptoms during manic and depressive episodes Prevent recurrence of manic and depressive episodes Do not worsen symptoms of mania or depression and do not accelerate the rate of cycling Antipsychotics Given during severe manic episodes Antidepressants
Given during depressive episodes Nondrug therapy Education – patient and family Psychotherapy – individual, group, and family Electroconvulsive therapy – last resort Drug selection Short-term therapy for manic episodes – lithium and valproate Short term therapy for depressive episodes – lithium or valproate, bupropion, venlafaxine, or an SSRI Long-term preventative treatment – antipsychotic agents Promoting adherence Short term hospitalization Long term prophylactic therapy Education for both patient and family Therapeutic uses Monitoring plasma lithium levels Drug interactions
Mood Stabilizing Drugs Lithium Low therapeutic index 0 to 1 mEq/L Adverse effects Excessive lithium levels Greater than 1 mEq/L Monitor levels every 2 to 3 days at initiation of therapy and ten every 3 to 6 months Therapeutic lithium levels Gastrointestinal effects Tremors Polyuria Renal toxicity Goiter and hypothyroidism Teratogenesis Chemistry Simple inorganic ions Found naturally in animal tissues Therapeutic uses BPD Alcoholism Bulimia Schizophrenia Glucocorticoid-induced psychosis Drug interactions Diuretics NSAIDs
Pharmacology Exam 4 Study Guide
Course: Pharmacology (NSG 124)
University: Herzing University

- Discover more from: