- Information
- AI Chat
Saunders Maternity and Newborn Medications Nclex
Adult Health II (NUR 2211)
Hillsborough Community College
Recommended for you
Students also viewed
- HESI Advanced Clinical Concepts
- Fundamentals of Nursing - Ch. 49 Sensory Alterations - RN Nclex
- Fundamentals of Nursing - Ch. 42 Fluid, Electrolyte, and Acid-Base Balance - RN Nclex
- Saunders Fundamentals of Care RN Nclex
- Saunders Ch. 5 Cultural Awareness and Health Practices Nclex
- Saunders Complex Care RN Nclex 69
Preview text
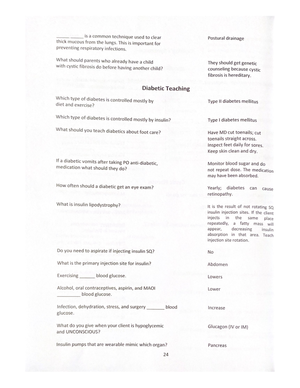
C H A P T E R 2 8
Maternity and Newborn Medications
evolve.elsevier/Silvestri/comprehensiveRN/
Priority Concepts
Health Promotion, Safety
The Food and Drug Administration has initiated the Pregnancy and Lactation Labeling Rule (PLLR). This is a revision to the previous system that used Category A, B, C, D, and X. The PLLR provides more information on the risks and benefits of using medications during pregnancy. The PLLR also provides more information to assist the provider and pregnant mother to make informed decisions together, so as to not deter medication use during pregnancy when it is necessary.
I. Tocolytics A. Description: Tocolytics are medications that produce uterine relaxation and suppress uterine activity (Table 28-1). B. Uses: To halt uterine contractions and prevent preterm birth; dihydropyridine calcium channel blockers such as nifedipine and magnesium sulfate may be prescribed to achieve this goal. Terbutaline is another medication used for this effect. C. Adverse effects and contraindications 1. See Table 28-1 for a description of adverse effects. 2. Maternal contraindications include severe preeclampsia and eclampsia, active vaginal bleeding, intrauterine infection, cardiac disease, placental abruption, or poorly controlled diabetes. 3. Fetal contraindications include estimated gestational age greater than 37 weeks, cervical dilation greater than 4 cm, fetal demise, lethal fetal anomaly, chorioamnionitis, acute fetal distress, and chronic intrauterine growth restriction.
D. Interventions for the client receiving tocolytic therapy
- Position the client on her side to enhance placental perfusion and reduce pressure on the cervix.
- Monitor maternal vital signs, fetal status, and labor status frequently according to agency protocol.
- Monitor for signs of adverse effects to the medication.
- Monitor daily weight and input and output status, and
provide fluid intake as prescribed. 5. Offer comfort measures and provide psychosocial support to the client and family. 6. See Table 28-1 for interventions specific to each tocolytic medication.
II. Magnesium Sulfate
A. Description (Table 28-1) 1. Magnesium sulfate is a central nervous system depressant and antiseizure medication. 2. The medication causes smooth muscle relaxation.
- The antidote is calcium gluconate.
B. Uses 1. Stopping preterm labor to prevent preterm birth, although it is less commonly used for this effect in practice 2. Preventing and controlling seizures in preeclamptic and eclamptic clients
C. Adverse effects and contraindications
- Magnesium sulfate can cause respiratory depression, depressed reflexes, flushing, hypotension, extreme muscle weakness, decreased urine output, pulmonary edema, and elevated serum magnesium levels.
- Continuous intravenous (IV) infusion increases the risk of magnesium toxicity in the newborn.
- Magnesium sulfate is stopped for delivery only if the mother is having a C-section.
- Magnesium sulfate may be prescribed for the first 12 to 24 hours postpartum if it is used for preeclampsia.
- High doses can cause loss of deep tendon reflexes, heart block, respiratory paralysis, and cardiac arrest.
- The medication is contraindicated in clients with heart block, myocardial damage, or kidney failure.
- The medication is used with caution in clients with kidney impairment.
D. Interventions
Monitor maternal vital signs, especially respirations, every 30 to 60 minutes.
Assess renal function and electrocardiogram for cardiac function.
Monitor magnesium levels every 6 hours or if signs and symptoms of toxicity are noted—the target range when used as a tocolytic agent is 4 to 7 mEq/L (2 to 3 mmol/L); if the magnesium level increases, notify
Monitor mother for signs of infection.
Monitor white blood cell count.
Monitor blood glucose levels.
Administer by deep intramuscular injection. IV. Opioid Analgesics A. Description
Used to relieve moderate to severe pain associated with labor
Administered by intramuscular or IV route
Regular use of opioids during pregnancy may
produce withdrawal symptoms in the newborn (irritability, excessive crying, tremors, hyperactive reflexes, fever, vomiting, diarrhea, yawning, sneezing, and seizures).
- Antidotes for opioids
a. Naloxone is usually the treatment of choice because it rapidly reverses opioid toxicity; the dose may need to be repeated every few hours until opioid concentrations have decreased to nontoxic levels. b. These medications can cause withdrawal in opioid-dependent clients. B. Hydromorphone hydrochloride
- Can cause dizziness, nausea, vomiting, sedation, decreased blood pressure, decreased respirations, diaphoresis, flushed face, and urinary retention
- May be prescribed to be administered with an antiemetic such as promethazine to prevent nausea
- High dosages may result in respiratory depression, skeletal muscle flaccidity, cold clammy skin, cyanosis, and extreme somnolence progressing to seizures, stupor, and coma.
- Used cautiously in clients delivering preterm newborns
- Not administered in advanced labor (typically once transition phase during stage 1 of labor has been reached); if the medication is not adequately removed from the fetal circulation, respiratory depression can occur. C. Fentanyl and sufentanil can cause respiratory depression, dizziness, drowsiness, hypotension, urinary retention, and fetal narcosis and distress; sufentanil is used less commonly than fentanyl.
D. Butorphanol tartrate and nalbuphine 1. May be prescribed depending on OB preference 2. Can cause confusion, sedation, sweating, nausea, vomiting, hypotension, and sinusoidal-like fetal heart rhythm 3. Use with caution in a client with preexisting opioid dependency, because these medications can precipitate withdrawal symptoms in the client and the newborn.
E. Interventions
- Monitor vital signs, particularly respiratory status; if respirations are 12 breaths per minute or less, withhold the medication and contact the OB.
- Monitor the fetal heart rate and characteristics of uterine contractions.
- Monitor for blood pressure changes (hypotension); maintain the client in a recumbent position (elevate the hip with a wedge pillow or other device).
- Record the level of pain relief.
- Monitor the bladder for distention and retention.
- Have the antidote naloxone readily accessible, especially if delivery is expected to occur during peak medication absorption time.
Obtain a medication history before the administration of an
opioid analgesic. Some medications may be contraindicated if the client has a history of opioid dependency, because these medications can precipitate withdrawal symptoms in the client and newborn. V. Prostaglandins (Box 28-1) A. Description
- Ripen the cervix, making it softer and causing it to begin to dilate and efface
- Stimulate uterine contractions
- Administered vaginally B. Uses
- Preinduction cervical ripening (ripening of the cervix before the induction of labor when the Bishop score is ≤ 4)
- Induction of labor
- Induction of abortion (abortifacient agent)
C. Adverse effects and contraindications
Gastrointestinal effects, including diarrhea, nausea, vomiting, and stomach cramps
Fever, chills, flushing, headache, and hypotension
Manages an incomplete abortion
C. Adverse effects and contraindications
- Adverse effects include allergies, dysrhythmias, changes in blood pressure, uterine rupture, and water intoxication.
- Oxytocin may produce uterine hypertonicity, resulting in fetal or maternal adverse effects.
- High doses may cause hypotension, with rebound hypertension.
- Postpartum hemorrhage can occur and should be monitored for, because the uterus may become atonic when the medication wears off.
- Oxytocin should not be used in a client who cannot deliver vaginally or in a client with hypertonic uterine contractions; it is also contraindicated in a client with active genital herpes.
D. Interventions
Monitor maternal vital signs (every 15 minutes), especially the blood pressure and heart rate, weight, intake and output, level of consciousness, and lung sounds.
Monitor frequency, duration, and force of contractions and resting uterine tone every 15 minutes.
Monitor fetal heart rate every 15 minutes, and notify the OB if significant changes occur; use of an internal fetal scalp electrode may be prescribed.
Administered by IV infusion via an infusion monitoring device (most common route); prescribed additive solution is piggybacked at the port nearest the point of venous insertion (prescribed additive solution may be normal saline, lactated Ringer’s, or 5% dextrose in water).
Carefully monitor the dose being administered; do not leave the client unattended while the oxytocin is infusing.
Administer oxygen if prescribed.
Monitor for hypertonic contractions or a nonreassuring fetal heart rate and notify the OB if these occur (see Priority Nursing Actions).
Stop the medication if uterine hyperstimulation or a nonreassuring fetal heart rate occurs; turn the client on her side, increase the IV rate of the prescribed additive solution, and administer oxygen via face mask.
Monitor for signs of water intoxication.
Have emergency equipment readily accessible.
Document the dose of the medication and the time the medication was started, increased, maintained, and discontinued; document the client’s response.
Keep the client and family informed of the client’s progress.
Calculating an oxytocin drip (Box 28-3)
P r ior ity Nur sing Actions
Hypertonic Contractions or a Nonreassuring Fetal Heart Rate during Oxytocin Infusion 1. Stop the oxytocin infusion. 2. Turn the client on her side, stay with the client, and ask another nurse to contact the obstetrician (OB). 3. Increase the flow rate of the intravenous (IV) solution that does not contain the oxytocin. 4. Administer oxygen, 8 to 10 L/minute, by snug face mask. 5. Assess maternal vital signs; fetal heart rate and patterns; and frequency, duration, and force of contractions. 6. Document the event, actions taken, and the response.
Reference
Lowdermilk et al. (2016), p. 784.
VII. Medications Used to Manage Postpartum Hemorrhage (Box 28-4) A. Ergot alkaloid 1. Description a. Methylergonovine maleate is an ergot alkaloid. b. Directly stimulates uterine muscle, increases the force and frequency of contractions, and produces a firm tetanic contraction of the uterus
c. Can produce arterial
vasoconstriction and vasospasm of the coronary arteries d. An ergot alkaloid is administered postpartum and is not administered before the birth of the placenta. 2. Uses a. Postpartum hemorrhage b. Postabortal hemorrhage resulting from atony or involution 3. Adverse effects and contraindications
a. Can cause nausea, uterine
- Adverse effects and contraindications a. Can cause headache, nausea, vomiting, diarrhea, fever, tachycardia, and hypertension b. Contraindicated if the client has asthma
- Interventions a. Monitor vital signs. b. Monitor vaginal bleeding and uterine tone. C. Oxytocin: See Section VI on uterine stimulants. VIII. Rho(D) Immune Globulin
A. Description 1. Prevention of anti-Rho(D) antibody formation is most successful if the medication is administered twice, at 28 weeks’ gestation and again within 72 hours after delivery.
- Rho(D) immune globulin also should be
administered within 72 hours after potential or actual exposure to Rh-positive blood and must be given with each subsequent exposure or potential exposure to Rh-positive blood. B. Use: To prevent isoimmunization in Rh-negative clients who are negative for Rh antibodies and exposed or potentially exposed to Rh-positive red blood cells by amniocentesis, chorionic villus sampling, transfusion, termination of pregnancy, abdominal trauma, or bleeding during pregnancy or the birth process C. Adverse effects and contraindications
- Elevated temperature
- Tenderness at the injection site
- Contraindicated for Rh-positive clients
- Contraindicated in clients with a history of systemic allergic reactions to preparations containing human immunoglobulins
- Note: Not administered to a newborn
D. Interventions
- Administer to the client by intramuscular injection at 28 weeks’ gestation and within 72 hours after delivery.
- Never administer by the IV route.
- Monitor for temperature elevation.
- Monitor injection site for tenderness.
Rho(D) immune globulin is of no benefit when the client has
developed a positive antibody titer to the Rh antigen.
IX. Rubella Vaccine
A. Given subcutaneously before hospital discharge to a nonimmune postpartum client B. Administered if the rubella titer is less than 1: C. Adverse effects: Transient rash, hypersensitivity D. Contraindicated in a client with a hypersensitivity to eggs (check with the OB regarding administration) E. Interventions 1. Assess for allergy to duck eggs and notify the OB before administration if an allergy exists. 2. Question administration if the client or other family members are immunocompromised.
The client should avoid pregnancy for 1 to 3 months (or as
prescribed) after immunization with rubella vaccine. Inform the client about the need to use a contraception method during this time. X. Lung Surfactants A. Description
- Replenish surfactant and restore surface activity to the lungs to prevent and treat respiratory distress syndrome.
- Administered to the newborn by the intratracheal route. B. Use: To prevent or treat respiratory distress syndrome in premature newborns C. Adverse effects and contraindications
- Adverse effects include transient bradycardia and oxygen desaturation; pulmonary hemorrhage, mucus plugging, and endotracheal tube reflux can also occur.
- Surfactants are administered with caution in newborns at risk for circulatory overload.
D. Interventions
- Instill surfactant through the catheter inserted into the newborn’s endotracheal tube; avoid suctioning for at least 2 hours after administration.
- Monitor for bradycardia and decreased oxygen saturation during administration.
- Monitor respiratory status and lung sounds and for signs of adverse effects. XI. Eye Prophylaxis for the Newborn
A. Description
- Preventive eye treatment against ophthalmia neonatorum in the newborn is required by law in the
C. Adverse effects: Rash, fever, erythema, and pain at injection site
D. Interventions
Parental consent must be obtained.
Administer intramuscularly in the lateral aspect of the middle third of the vastus lateralis muscle.
If the infant was born to a mother positive for hepatitis B surface antigen, hepatitis B immune globulin should be given within 12 hours of birth in addition to hepatitis B vaccine. Then follow the regularly scheduled hepatitis B vaccination schedule.
Document immunization administration on a vaccination card so that the parents have a record that the vaccine was administered. XIV. Contraceptives A. Description
These medications contain a combination of estrogen and a progestin or a progestin alone and come in several different forms, including oral and intramuscular preparations and implants.
Estrogen-progestin combinations suppress ovulation and change the cervical mucus, making it difficult for sperm to enter.
Medications that contain only progestins are less effective than the combined medications.
Contraceptives usually are taken for 21
consecutive days and stopped for 7 days; the administration cycle is then repeated. 5. Contraceptives provide reversible prevention of pregnancy. 6. Contraceptives are useful in controlling irregular or excessive menstrual cycles.
- Risk factors associated with the development
of complications related to the use of contraceptives include smoking, obesity, and hypertension.
- Contraceptives are contraindicated in women
with hypertension, thromboembolic disease, cerebrovascular or coronary artery disease, estrogen- dependent cancers, and pregnancy.
- Contraceptives should be avoided with the use
of hepatotoxic medications. 10. Contraceptives interfere with the activity of
bromocriptine mesylate and anticoagulants and increase the toxicity of tricyclic antidepressants. 11. Contraceptives may alter blood glucose levels. 12. Antibiotics may decrease the absorption and effectiveness of oral contraceptives. B. Side and adverse effects
- Breakthrough bleeding
- Excessive cervical mucus formation
- Breast tenderness
- Hypertension
- Nausea, vomiting
C. Interventions
Monitor vital signs and weight.
Instruct the client in the administration of the medication (it may take up to 1 week for full contraceptive effect to occur when the medication is begun).
Instruct the client with diabetes mellitus to monitor blood glucose levels carefully.
Instruct the client to report signs of thromboembolic complications.
Instruct the client to notify the OB if vaginal bleeding or menstrual irregularities occur or if pregnancy is suspected.
Advise the client to use an alternative method of birth control when taking antibiotics because these may decrease absorption of the oral contraceptive.
Instruct the client to perform breast self-examination regularly and about the importance of annual physical examinations.
Contraceptive patches a. Designed to be worn for 3 weeks and removed for a 1-week period b. Applied on clean, dry, intact skin on the buttocks, abdomen, upper outer arm, or upper torso c. Instruct the client to peel away half of the backing on a patch, apply the sticky surface to the skin, remove the other half of the backing, and then press down on the patch with the palm for 10 seconds. d. Instruct the client to change the patch weekly, using a new location for each patch.
Risk of multiple births and birth defects
Ovarian overstimulation (abdominal pain,
distention, ascites, pleural effusion) 3. Headache, irritability 4. Fluid retention and bloating 5. Nausea, vomiting 6. Uterine bleeding 7. Ovarian enlargement 8. Gynecomastia 9. Rash 10. Orthostatic hypotension 11. Febrile reactions
C. Interventions
- Instruct the client regarding administration of the medication.
- Provide a calendar of treatment days and instructions on when intercourse should occur to increase therapeutic effectiveness of the medication.
- Provide information about the risks and hazards of multiple births.
- Instruct the client to notify the OB if signs of ovarian overstimulation occur.
- Inform the client about the need for regular follow-up for evaluation.
Table 28-
Tocolytics
Medication, Classification, and Actions Adverse Effects InterventionsNursing Terbutaline—selective beta 2 agonist that suppresses preterm labor by activating beta 2 receptors in the uterus—decreases both frequency and intensity of contractions; primarily used to delay birth for several hours to allow the fetus to mature more before being born
Maternal—Pulmonary edema, hypotension, hyperglycemia, and tachycardia
Administered by injection under the skin
Fetus—Tachycardia Dosing should stop after 48 hours and should be interrupted if the maternal heart rate exceeds 120 beats per minute Magnesium sulfate—central nervous system depressant; relaxes smooth muscle, including the uterus; used to halt preterm labor contractions;
Maternal—depressed respirations, depressed DTRs, hypotension, extreme muscle weakness, flushing,
Always use intravenous controller device for
used for preeclamptic clients to prevent seizures decreased urine output, pulmonary edema, serum magnesium levels > 7 mEq/L (3 mmol/L)
administration
Fetus—hypotonia and sleepiness Follow agency protocol for administration Discontinue infusion and notify OB if adverse effects occur Monitor for respirations < 12/min, urine output < 100 mL/4 hr (25-30 mL/hr) Monitor DTRs Monitor magnesium levels and report values outside therapeutic range of 4 to 7 mEq/L (2 to 3 mmol/L) Keep calcium gluconate readily accessible (antidote) Nifedipine-calcium channel blocker; relaxes smooth muscles, including the uterus, by blocking calcium entry; in some health care agencies, this may be the first-line agent to halt preterm labor contractions
Maternal—tachycardia, hypotension, dizziness, headache, nervousness, facial flushing, fatigue, nausea Fetus—May cause vascular dilation
Follow agency protocol for administration Use with magnesium sulfate is avoided because severe hypotension can occur Monitor for adverse effects
DTRs, Deep tendon reflexes; OB, obstetrician.
Table 28-
Assessing Deep Tendon Reflexes
Grade Deep Tendon Reflex Response 0 No response 1 Sluggish or diminished 2 Active or expected response 3 More brisk than expected, slightly hyperactive 4 Brisk, hyperactive, with intermittent or transient clonus
Data from Seidel H, Ball J, Dains J, Flynn J, Solomon B, Stewart R: Mosby’s guide to physical examination, ed 6, St. Louis, 2011, Mosby.
Box 28-
Prostaglandins
How many mU are in 1 U? There are 1000 mU in 1 U. If there are 1000 mU in 1 U, how many units in 2 mU? Answer: 0 U in 2 mU Now use the standard formula for calculation.
Now, determine how many milliliters should be given in 1 hour if the prescription is for 0 mL/minute. 0 mL/minute × 60 minutes (1 hour) = 6 mL/hr Note: Many electronic pumps allow for programming in units or milliunits per minute, eliminating the need to calculate the milliliters per hour, and this practice is recommended if available because medications are programmed in the pumps with dosage safeguards. If a dose that is too low or too high is programmed into the pump, the pump will flag or will not allow the nurse to proceed with administration.
Reference: Burcham & Rosenthal (2016), p. 782.
Box 28-
Medications Used to Manage Postpartum
Hemorrhage
▪ Methylergonovine ▪ Oxytocin ▪ Prostaglandin F2α: Carboprost tromethamine
Box 28-
Fertility Medications
▪ Chorionic gonadotropin ▪ Clomiphene citrate ▪ Follitropin alfa ▪ Follitropin beta ▪ Menotropins ▪ Urofollitropin ▪ Cetrorelix ▪ Ganirelix
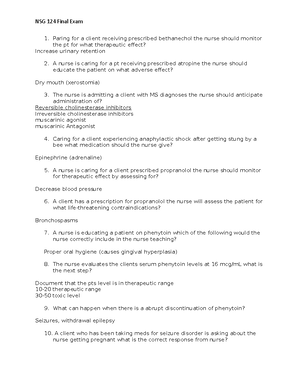
Practice Questions
The nurse is monitoring a client who is receiving oxytocin to induce labor. Which assessment findings should cause the nurse to immediately discontinue the oxytocin infusion? Select all that apply.
- Fatigue
Drowsiness
Uterine hyperstimulation
Late decelerations of the fetal heart rate
Early decelerations of the fetal heart rate
A pregnant client is receiving magnesium sulfate for the management of preeclampsia. The nurse determines that the client is experiencing toxicity from the medication if which findings are noted on assessment? Select all that apply.
Proteinuria of 3 +
Respirations of 10 breaths per minute
Presence of deep tendon reflexes
Urine output of 20 mL in an hour
Serum magnesium level of 4 mEq/L (2 mmol/L)
The nurse asks a nursing student to describe the procedure for administering erythromycin ointment to the eyes of a newborn. Which student statement indicates that further teaching is needed about administration of the eye medication?
“I will flush the eyes after instilling the ointment.”
“I will clean the newborn’s eyes before instilling ointment.”
“I need to administer the eye ointment within 1 hour after delivery.”
“I will instill the eye ointment into each of the newborn’s
Saunders Maternity and Newborn Medications Nclex
Course: Adult Health II (NUR 2211)
University: Hillsborough Community College

- Discover more from:
Recommended for you
Students also viewed
- HESI Advanced Clinical Concepts
- Fundamentals of Nursing - Ch. 49 Sensory Alterations - RN Nclex
- Fundamentals of Nursing - Ch. 42 Fluid, Electrolyte, and Acid-Base Balance - RN Nclex
- Saunders Fundamentals of Care RN Nclex
- Saunders Ch. 5 Cultural Awareness and Health Practices Nclex
- Saunders Complex Care RN Nclex 69