- Information
- AI Chat
Saunders Vital Signs and Laboratory Reference Intervals RN Nclex
Adult Health II (NUR 2211)
Hillsborough Community College
Recommended for you
Students also viewed
- Saunders Parenteral Nutrition RN Nclex
- Saunders Acid-Base Balance RN Nclex
- Saunders Ch. 6 Ethical and Legal Issues RN Nclex
- Saunders 7th Edition Integumentary Disorders of the Adult Client : Integumentary System RN Nclex
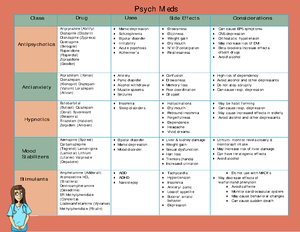
- Saunders Psychiatric Medications RN Nclex 68
- Saunders Foundations of Mental Health Nursing RN Nclex 64
Preview text
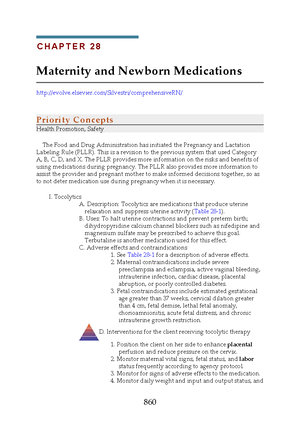
C H A P T E R 10
Vital Signs and Laboratory Reference Intervals
PRIORITY CONCEPTS Cellular Regulation; Perfusion
CRITICAL THINKING What Should You Do?
The nurse has just received a client from the postanesthesia care unit (PACU) and is monitoring the client’s vital signs. On arrival to the unit, the client’s temperature was 37 °C (98 °F) orally, the blood pressure was 142/ 78 mm Hg, the heart rate was 98 beats per minute, the respiratory rate was 14 breaths per minute, and the oxygen saturation was 95% on 3 L of oxygen via nasal cannula. The nurse returns to the room 30 minutes later to find the client’s temperature to be 36 °C (98 °F) orally, the blood pressure 95/ 54 mm Hg, the heart rate 118 beats per minute, the respiratory rate 18 breaths per minute, and the oxygen saturation 92% on 3 L of oxygen via nasal cannula. On the basis of these data, what actions should the nurse take? Answer located on p. 119.
I. Vital Signs
A. Description: Vital signs include tem perature, pulse,
respirations, blood pressure (BP), oxygen saturation (pulse oxim etry), and pain assessm ent.
B. Guidelines for m easuring vital signs
- Initial m easurem ent of vital signs provides base- line data on a client’s health status and is used to help identify changes in the client’s health status.
- Som e vital sign m easurem ents (tem perature, pulse, respirations, BP, pulse oxim etry) m ay be delegated to unlicensed assistive personnel (UAP), but the nurse is responsible for interpret- ing the findin gs.
- The nurse collaborates with the health care pro- vider (HCP) in determ ining the frequency of vital sign assessm ent and also m akes indepen- dent decisions regardin g their frequency on the basis of the client’s status. The nurse always documents vital sign measure- ments and reports abnormal findings to the HCP.
C. When vital signs are m easured
- On initial contact with a client (e., when a cli- ent is adm itted to a health care facility)
- Durin g physical assessm ent of a clien t
- Before and after an invasive diagnostic procedure or surgical procedure
- Durin g the adm inistration of m edication that affects the cardiac, respiratory, or tem perature- controlling fun ctions (e., in a client who has a fever); m ay be required before, during, and after adm inistration of the m edication
- Before, during, and after a blood transfusion
- Whenever a client’s condition changes
- Whenever an intervention (e., am bulation) m ay affect a clien t’s condition
- When a fever or known infection is present (every 2 to 4 hours)
II. Temperature
A. Description
- Norm al body tem perature ranges from 36° to 37° Celsius (C) (97° to 99° Fahrenh eit [F]); the average in a health y young adult is 37 °C (98 °F).
- Com m on m easurem ent sites are the m outh, rec- tum , axilla, ear, and across the forehead (tem po- ral artery site); various types of electronic m easuring devices are com m only used.
- Rectal tem peratures are usually 1 °F (0 °C) higher and axillary tem peratures about 1 °F (0 °C) lower than the norm al oral tem perature.
- Know how to convert a tem perature to a Fahren- heit or Celsius value (Box 10-1).
B. Nursing considerations
- Tim e of day a. Tem perature is generally in the low-norm al range at the tim e of awakening as a result of m uscle inactivity. b. Aftern oon body tem perature m ay be high- norm al as a result of the m etabolic process, activity, and environ m ental tem perature.
108
- Environm en tal tem perature: Body tem perature is lower in cold weath er and higher in warm weather.
- Age: Tem perature m ay fluctuate during the first year of life because the infant’s heat-regulating m ech anism is not fully developed.
- Physical exercise: Use of the large m uscles creates heat, causing an increase in body tem perature.
- Menstrual cycle: Tem perature decreases sligh tly just before ovulation but m ay increase to 1 °F above norm al during ovulation.
- Pregnancy: Body tem perature m ay consisten tly stay at high-n orm al because of an increase in the wom an’s m etabolic rate.
- Stress: Em otions increase horm on al secretion, leading to increased heat production and a higher tem perature.
- Illness: In fective agents and the inflam m atory response m ay cause an increase in tem perature.
- The inability to obtain a tem perature should not be ignored because it could represent a condition of hypotherm ia, a life-threatening condition in very young and older clients.
C. Methods of m easurem ent
- Oral a. If the client has recently consum ed hot or cold foods or liquids or has smoked or chewed gum , the nurse m ust wait 15 to 30 m inutes before taking the tem perature orally. b. The thermometer is placed under the tongue in 1 of the posterior sublingual pockets; ask the cli- ent to keep the tongue down and the lips closed and to not bite down on the thermometer.
- Rectal a. Place the clien t in the Sim s position. b. The tem perature is taken rectally when an accurate tem perature cannot be obtained orally or when the client has nasal conges- tion, has undergone nasal or oral surgery or had the jaws wired, has a nasogastric tube in place, is unable to keep the m outh closed, or is at risk for seizures. c. The therm om eter is lubricated and inserted into the rectum , toward the um bilicus, about 1 inch es (3 cm ) (no m ore than 0 inch [1 cm ] in an infant).
The temperature is not taken rectally in cardiac cli- ents; the client who has undergone rectal surgery; or the client with diarrhea, fecal impaction, or rectal bleeding or who is at risk for bleeding. 3. Axillary a. This m ethod of taking the tem perature is used when the oral or rectal tem perature m easure- m ent is contraindicated. b. Axillary m easurem ent is not as accurate as the oral, rectal, tym pan ic, or tem poral artery m ethod but is used when oth er m ethods of m easurem ent are not possible. c. The therm om eter is placed in the client’s dry axilla and the client is asked to hold the arm tightly against the chest, resting the arm on the chest; follow the instructions accom pan y- ing the m easurem ent device for the am ount of tim e the therm om eter should rem ain in the axillary area. 4. Tym panic a. The auditory canal is checked for the presence of redness, swelling, discharge, or a foreign body before the probe is inserted; the probe should not be inserted if the client has an inflam m atory condition of the auditory can al or if there is discharge from the ear. b. The reading m ay be affected by an ear infec- tion or excessive wax blockin g the ear canal. 5. Tem poral artery a. Ensure that the client’s forehead is dry. b. The therm om eter probe is placed flush against the skin and slid across the forehead or placed in the area of the tem poral artery and held in place. c. If the client is diaphoretic, the tem poral artery therm om eter probe m ay be placed on the neck, just behind the earlobe.
III. Pulse
A. Description
- The average adult pulse (heart) rate is 60 to 100 beats/ m in.
- Chan ges in pulse rate are used to evaluate the cli- ent’s tolerance of interven tions such as am bula- tion, bathing, dressing, and exercise.
- Pedal pulses are checked to determ ine whether the circulation is blocked in the artery up to that pulse point.
- When the pedal pulse is difficult to locate, a Doppler ultrasoun d stethoscope (ultrason ic stethoscope) m ay be needed to am plify the sounds of pulse waves.
B. Nursing considerations
- The heart rate slows with age.
- Exercise increases the heart rate.
- Em otion s stim ulate the sym path etic nervous sys- tem , increasing the heart rate.
BOX 10-1 Body Temperature Conversion
To convert Fahrenheit to Celsius: Degrees Fahrenheit – 32  5/ 9 ¼ Degrees Celsius Example: 98 °F – 32  5/ 9 ¼ 36 °C To convert Celsius to Fahrenheit: Degrees Celsius  9/ 5 + 32 ¼ Degrees Fahrenheit Example: 38 °C 9/ 5+ 32 ¼ 101 °F
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 109
- For an adult (age 18 and older), a norm al BP is a systolic pressure below 120 m m Hg and a dia- stolic pressure below 80 m m Hg.
- Classification s include prehypertension and stage 1 and stage 2 hypertension (Box 10-3).
- In postural (orthostatic) hypotension , a norm o- ten sive client exhibits sym ptom s and low BP on risin g to an upright position.
- To obtain orthostatic vital sign m easurem ents, check the BP and pulse with the client supine, sit- ting, and standing; readings are obtained 1 to 3 m inutes after the client changes position.
B. Nursing considerations
- Factors affecting BP a. BP tends to increase as the aging process progresses. b. Stress results in sym path etic stim ulation that increases the BP. c. The inciden ce of high BP is higher am on g African Am ericans than am ong Am ericans of European descent. d. Antih ypertensive m edications and opioid analgesics can decrease BP. e. BP is typically lowest in the early m orning, gradually increases during the day, and peaks in the late afternoon and evening. f. After puberty, m ales tend to have higher BP than fem ales; after m enopause, wom en ten d to have higher BP than m en of the sam e age.
- Guidelines for m easuring BP a. Determ ine the best site for assessm ent. b. Avoid applying a cuff to an extrem ity into which intravenous (IV) fluids are infusing, where an arteriovenous shunt or fistula is present, on the side on which breast or axil- lary surgery has been perform ed, or on an extrem ity that has been traum atized or is diseased. c. The leg m ay be used if the brach ial artery is inaccessible; the cuff is wrapped around the thigh and the stethoscope is placed over the popliteal artery. d. Ensure that the client has not sm oked or exer- cised in the 30 m inutes before m easurem ent because both activities can yield falsely high readings.
e. Have the clien t assum e a sitting (with feet flat on floor) or lying position and then rest for 5 m inutes before the m easurem ent; ask the client not to speak during the m easurem ent. f. Ensure that the cuff is fully deflated, then wrap it evenly and snugly around the extrem ity. g. Ensure that the steth oscope bein g used fits the exam iner and does not im pair hearin g. h. Docum ent the first Korotkoff sound at phase 1 (heard as the blood pulsates through the vessel when air is released from the BP cuff and pressure on the artery is reduced) as the systolic pressure and the beginning of the fifth Korotkoff soun d at phase 5 as the dia- stolic pressure. i. BP readings obtained electronically with a vital sign m onitoring m achine should be checked with a m anual cuff if there is any con- cern about the accuracy of the reading.
When taking a BP, select the appropriate cuff size; a cuff that is too small will yield a falsely high reading, and a cuff that is too large will yield a falsely low one.
VI. Pulse Oximetry
A. Description
- Pulse oxim etry is a nonin vasive test that registers the oxygen saturation of the clien t’s hem oglobin.
- The capillary oxygen saturation (SaO 2 ) is recorded as a percentage.
- The norm al value is 95% to 100%.
- After a hypoxic client uses up the readily avail- able oxygen (m easured as the arterial oxygen pressure, PaO 2 , on arterial blood gas [ABG] test- ing), the reserve oxygen , that oxygen attach ed to the hem oglobin (SaO 2 ), is drawn on to pro- vide oxygen to the tissues.
- A pulse oxim eter reading can alert the nurse to hypoxem ia before clinical signs occur.
- If pulse oxim etry readings are below norm al, instruct the client in deep breathing tech nique and recheck the pulse oxim etry.
B. Procedure
- A sensor is placed on the clien t’s finger, toe, nose, earlobe, or forehead to m easure oxygen satura- tion, which then is displayed on a m onitor.
- Maintain the tran sducer at heart level.
- Do not select an extrem ity with an im pedim ent to blood flow.
A usual pulse oximetry reading is between 95% and 100%. A pulse oximetry reading lower than 90% neces- sitates HCP notification; values below 90% are accept- able only in certain chronic conditions. Agency procedures and HCP prescriptions are followed regard- ing actions to take for specific readings.
BOX 10-3 Hypertension Classifications
Prehypertension: A systolic blood pressure (BP) of 120 to 139 mm Hg or a diastolic pressure of 80 to 89 mm Hg Stage 1: A systolic BP of 140 to 159 mm Hg or a diastolic pres- sure of 90 to 99 mm Hg Stage 2: A systolic BP equal to or greater than 160 mm Hg or a diastolic pressure equal to or greater than 100 mm Hg
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 111
VII. Pain
A. Types of pain
- Acute: Usually associated with an injury, m edical condition, or surgical procedure; lasts hours to a few days
- Chron ic: Usually associated with long-term or chron ic illnesses or disorders; m ay continue for m onth s or even years
- Phantom : Occurs after the loss of a body part (am putation ); m ay be felt in the am putated part for years after the am putation
B. Assessm ent
- Pain is a highly individual experience.
- Ask the client to describe pain in term s of degree, quality, area, and frequen cy.
- Ask the client about the use of com plem entary and alternative therapies to alleviate pain.
- Pain experienced by the older client m ay be m an- ifested differently than pain experienced by m em bers of other age groups (e., sleep distur- bances, changes in gait and m obility, decreased socialization, depression).
- Clients with cognitive disorders (e., a client with dem entia, a com atose clien t) m ay not be able to describe their pain experiences.
- The nurse should be alert to nonverbal indicators of pain (Box 10-4).
- Ask the client to use a num ber-based pain scale (a picture-based scale m ay be used in children or clients who cann ot verbally describe their pain) to rate the degree of pain (Fig. 10-1).
- Evaluate client response to nonpharm acological interven tions. Consider the client’s culture in assessing pain; some cultures, including many Asian cultures, frown on the outward expression of pain.
C. Conven tional nonph arm acological interventions
- Cutan eous stim ulation a. Techniques include heat, cold, and pressure and vibration. Therapeutic touch and m assage are also cutaneous stim ulation and m ay be considered complementary and alternative techniques.
b. Such treatm ents m ay require an HCP’s prescription. 2. Tran scutaneous electrical nerve stim ulation (TENS) a. TENS is also referred to as percutan eous elec- trical nerve stim ulation (PENS). b. This technique, which m ay require an HCP’s prescription, involves the application of a battery-operated device that delivers a low electrical current to the skin and underlying tissues to block pain. 3. Binders, slings, and oth er supportive devices a. Cloths or oth er m aterials or devices, wrapped around a lim b or body part, can ease the pain of strains, sprains, and surgical incisions. b. Such devices may require an HCP’s prescription. c. Elevation of the affected body part is another interven tion that can reduce swelling; sup- porting an extrem ity on a pillow m ay lessen discom fort. 4. Heat and cold a. The application of heat and cold or alternat- ing application of the two can soothe pain resultin g from m uscle strain. b. Such treatm ent m ay require an HCP’s pre- scription.
BOX 10-4 Nonverbal Indicators of Pain
▪ Moaning
▪ Crying
▪ Irritability
▪ Restlessness
▪ Grimacing or frowning
▪ Inability to sleep
▪ Rigid posture
▪ Increased blood pressure, heart rate, or respiratory rate
▪ Nausea
▪ Diaphoresis
0 No hurt
1 or 2 Hurts little bit
2 or 4 Hurts little more
3 or 6 Hurts e ve n more
4 or 8 Hurts whole lot
5 or 10 Hurts worst B
####### A
No pa in
0 1 2 3 4 5 6 7 8 9 10 S e ve re pa in
Nume ric al
De s c riptive
No pa in Mild pa in Mode ra te pa in
Unbe a ra ble pa in
S e ve re pa in
Vis ual analo g
No pa in Unbe a ra ble pa in Clie nts de s igna te a point on the s ca le corre s ponding to the ir pe rce ption of the pa in’s s e ve rity a t the time of a s s e s s me nt.
FIGURE 10-1 Pain assessment scales. A, Numerical, descriptive, and visual analog scales. B, Wong-Baker FACES® Pain Rating Scale. (B, Copy- right 1983, Wong-Baker FACES® Foundation, WongBakerFACES. Used with permission. Originally published in Whaley & Wong’s Nursing Care of Infants and Children. ©Elsevier Inc.)
112 UNIT III Nursing Sciences
The major concern with acetaminophen is hepatotoxicity.
B. Opioid analgesics
Description a. These m edication s suppress pain im pulses but can also suppress respiration and cough- ing by acting on the respiratory and cough center, located in the m edulla of the brain stem. b. Review the client’s history and note that cli- ents with im paired renal or liver function m ay only be able to tolerate low doses of opioid analgesics. c. Intraven ous route adm inistration produces a faster effect than other routes but the effect lasts shorter to relieve pain d. Opioids, which produce euphoria and seda- tion, can cause physical dependence. e. Adm in ister the m edication 30 to 60 m inutes before painful activities. f. Monitor the respiratory rate; if it is slower than 12 breaths/m in in an adult, withhold the m edication and notify the HCP. g. Monitor the pulse; if bradycardia develops, withh old the m edication and notify the HCP. h Monitor the BP for hypotension and assess before adm inistering pain m edications to decrease the risk of adverse effects. i. Auscultate the lungs for norm al breath sounds. j. Encourage activities such as turning, deep breath ing, and incentive spirom etry to help preven t atelectasis and pneum onia. k. Monitor the client’s level of consciousness. l. Initiate safety precautions. m. Monitor intake and output and assess the cli- ent for urine retention. n. Instruct the client to take oral doses with m ilk or a snack to reduce gastric irritation. o. Instruct the client to avoid activities that require alertness. p. Assess the effectiveness of the m edication 30 m inutes after adm instration. q. Have an opioid antagonist (e., naloxone), oxygen , and resuscitation equipm ent avail- able. An electronic infusion device is always used for con- tinuous or dose-demand IV infusion of opioid analgesics.
Codeine sulfate a. This m edication is also used in low doses as a cough suppressan t. b. It m ay cause constipation. c. Com m on m edications in this class are hydro- codon e and oxycodone (synth etic form s).
Hydrom orphon e a. The prim ary concern is respiration depres- sion. b. Other effects include drowsin ess, dizzin ess, and orthostatic hypoten sion. c. Monitor vital signs, especially the respiratory rate and BP.
Morph ine sulfate a. Morph ine sulfate is used to ease acute pain resultin g from m yocardial infarction or can- cer, for dyspnea resultin g from pulm onary edem a, and as a preoperative m edication. b. The m ajor concern is respiratory depression, but postural hypoten sion, urine retention, constipation, and pupillary constriction m ay also occur; m onitor the client for adverse effects. c. Morph ine m ay cause nausea and vom iting by increasing vestibular sensitivity. d. It is contraindicated in severe respiratory dis- orders, head injuries, severe renal disease, or seizure activity, and in the presence of increased intracran ial pressure. e. Monitor the client for urine retention. f. Monitor bowel sounds for decreased peristal- sis; constipation m ay occur. g. Monitor the pupil for changes; pinpoint pupils m ay indicate overdose.
IX. Laboratory Reference Intervals
For reference throughout the chapter, see Figure 10-2.
A. Methods for drawin g blood (Table 10-1)
B. Serum sodium
- A m ajor cation of extracellular fluid.
- Maintains osm otic pressure and acid-base bal- ance, and assists in the transm ission of nerve im pulses.
- Is absorbed from the sm all intestine and excreted in the urine in am ounts dependent on dietary intake.
- Norm al reference interval: 135 to 145 m Eq/L (135 to 145 m m ol/L). Drawing blood specimens from an extremity in which an IV solution is infusing can produce an inaccu- rate result, depending on the test being performed and the type of solution infusing. Prolonged use of a tourni- quet before venous sampling can increase the blood level of potassium, producing an inaccurate result.
C. Serum potassium
- A m ajor intracellular cation , potassium regulates cellular water balan ce, electrical conduction in m uscle cells, and acid-base balance.
- The body obtains potassium through dietary ingestion and the kidneys preserve or excrete potassium , depending on cellular need.
114 UNIT III Nursing Sciences
TOTAL BODY WEIGHT
WHOLE BLOOD (pe rce nta ge by volume )
PLAS MA (pe rce nta ge by we ight) Blood 8%
Othe r fluids a nd tis s ue s 92%
Ce ntrifuge d s a mple of blood
Buffy coa t
PLAS MA 55%
Albumins Globulins Fibrinoge n P rothrombin
54% 38% 4% 1%
PROTEINS
Ga s e s Ions Nutrie nts
Re gula tory s ubs ta nce s Wa s te products
OTHER S OLUTES
LEUKOCYTES FORMED ELEMENTS 45%
P la te le ts
P rote ins
Wa te r
Othe r s olute s
7%
91%
2%
Ne utrophils 60-70%
Lymphocyte s 20-25%
Monocyte s 3-8%
Eos inophils 2-4%
Ba s ophils 0-1%
150,000-400,000 mm 3 (150-400 × 109 /L) White blood ce lls
5000-10,000 mm 3 (5.0-10 × 109 /L)
FORMED ELEMENTS
FIGURE 10-2 Approximate values for the components of blood in a normal adult.
TABLE 10-1 Obtaining a Blood Sample
Venipuncture Peripheral Intravenous Line Central Intravenous Line Check health care provider’s (HCP’s) prescription.
Check HCP’s prescription. Check HCP’s prescription.
Identify foods, medications, or other factors that may affect the procedure or results.
Identify foods, medications, or other factors such as the type of solution infusing that may affect the procedure or results.
Identify foods, medications, or other factors such as the type of solution infusing that may affect the procedure or results. Gather needed supplies, including gloves, needle (appropriate gauge and size), transfer/ collection device per agency policy, specimen containers per agency policy, tourniquet, antiseptic swabs, 2 Â 2 inch gauze, tape, tube label(s), biohazard bag, requisition form or bar code per agency policy.
Gather needed supplies, including gloves, tourniquet, transparent dressing or other type of dressing, tape, 2 Â 2 inch gauze, antiseptic agent, extension set (optional), two 5- or 10-mL normal saline flushes, one empty 5- or 10-mL syringe (depending on the amount of blood needed), transfer/ collection device per agency policy, specimen containers per agency policy, alcohol- impregnated intravenous (IV) line end caps, tube labels, biohazard bag, requisition form or bar code per agency policy.
Gather needed supplies, including gloves, transfer/ collection device per agency policy, specimen containers per agency policy, two 5- or 10-mL normal saline flushes, one empty 5- or 10-mLsyringe (depending on the amount of blood needed), antiseptic swabs, alcohol- impregnated IV line end caps, 2 masks, biohazard bag, requisition form or bar code per agency policy.
Perform hand hygiene. Identify the client with at least 2 accepted identifiers.
Perform hand hygiene. Identify the client with at least 2 accepted identifiers.
Perform hand hygiene. Identify the client with at least 2 accepted identifiers. Explain the purpose of the test and procedure to the client.
Explain the purpose of the test and procedure to the client.
Explain the purpose of the test and procedure to the client. Apply clean gloves. Place the client in a lying position or a semi-Fowler’s position. Place a small pillow or towel under the extremity.
Prepare extension set if being used by priming with normal saline. Attach syringe to extension set. Place extension set within reach while maintaining aseptic technique and keeping it in the package.
Place mask on self and client or ask client to turn the head away. Stop anyrunning infusions for at least 1 minute.
Apply tourniquet 5 to 10 cm above the venipuncture site so it can be removed in 1 motion.
Apply tourniquet 10 to 15 cm above intravenous site. Clamp all ports. Scrub port to be used with antiseptic swab.
Ask the client to open and close the fist several times, then clench the fist.
Apply gloves. Scrub tubing insertion port with antiseptic solution or per agency policy.
Attach 5- or 10-mL normal saline flush and unclamp line. Flush line with appropriate amount per agency policy and withdraw 5- 10 mL of blood to discard (per agency policy). Clamp line and detach flush. Continued
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 115
- A PT value within 2 secon ds (plus or m inus) of the control is considered norm al.
- The INR is a frequently used test to m easure the effects of som e anticoagulants.
- The INR standardizes the PT ratio and is calcu- lated in the laboratory setting by raising the observed PT ratio to the power of the intern a- tional sensitivity index specific to the throm bo- plastin reagent used.
- If a PT is prescribed, baseline specim en should be drawn before anticoagulation therapy is started; note the tim e of collection on the labora- tory form.
- Provide direct pressure to the venipuncture site for 3 to 5 m inutes.
- Con current warfarin therapy with heparin ther- apy can length en the PT for up to 5 hours after dosin g.
- Diets high in green leafy vegetables can increase the absorption of vitam in K, which shortens the PT.
- Orally adm inistered anticoagulation therapy usually m aintains the PT at 1 to 2 tim es the lab- oratory control value.
- Norm al reference intervals a. PT: 11 to 12 secon ds (conven tional and SI units) b. INR: 2 to 3 for standard warfarin therapy c. INR: 3 to 4 for high-dose warfarin therapy Ifthe PTvalue is longer than 32 seconds and the INRis greater than 3 in a client receiving standard warfarin ther- apy (or per agency policy), initiate bleeding precautions.
F. Platelet coun t
- Platelets function in hem ostatic plug form ation , clot retraction, and coagulation factor activation. 2 Platelets are produced by the bone m arrow to fun ction in hem ostasis.
- Normal reference interval: 150,000-400,000 m m 3 (150–400 Â 10 9 /L)
- Mon itor the venipuncture site for bleeding in cli- en ts with known throm bocytopenia.
- High altitudes, chron ic cold weather, and exer- cise increase platelet counts.
- Bleeding precaution s should be instituted in cli- en ts when the platelet count falls sufficien tly below the norm al level; the specific value for im plem en ting bleeding precaution s usually is determ ined by agency policy.
Monitor the platelet count closely in clients receiv- ing chemotherapy because of the risk for thrombocyto- penia. In addition, any client who will be having an invasive procedure (such as a liver biopsy or thoracen- tesis) should have coagulation studies and platelet counts done before the procedure.
G. Hem oglobin and hem atocrit
- Hem oglobin is the m ain com ponent of erythro- cytes and serves as the vehicle for transporting oxygen and carbon dioxide.
- Hem atocrit represents red blood cell (RBC) m ass and is an im portant m easurem ent in the pres- ence of anem ia or polycythem ia (Table 10-2).
- Fasting is not required for this test.
H. Lipids
- Blood lipids consist prim arily of cholesterol, tri- glycerides, and phospholipids.
- Lipid assessm ent includes total cholesterol, high- density lipoprotein (HDL), low-density lipopro- tein (LDL), and triglycerides.
- Cholesterol is present in all body tissues and is a m ajor com ponen t of LDLs, brain and nerve cells, cell m em branes, and som e gallbladder ston es.
- Triglycerides constitute a m ajor part of very low- density lipoproteins and a sm all part of LDLs.
- Triglycerides are synthesized in the liver from fatty acids, protein , and glucose, and are obtained from the diet.
- Increased cholesterol levels, LDL levels, and tri- glyceride levels place the client at risk for coro- nary artery disease.
- HDL helps to protect against the risk of coronary artery disease.
- Oral contraceptives m ay increase the lipid level.
- Instruct the clien t to abstain from food and fluid, except for water, for 12 to 14 hours and from alcohol for 24 hours before the test.
- Instruct the client to avoid consum ing high- cholesterol foods with the even ing m eal before the test.
- Norm al referen ce intervals (Table 10-3).
I. Fasting blood glucose
- Glucose is a m on osaccharide foun d in fruits and is form ed from the digestion of carbohydrates and the conversion of glycogen by the liver.
- Glucose is the m ain source of cellular energy for the body and is essential for brain and erythro- cyte fun ction.
TABLE 10-2 Hemoglobin and Hematocrit: Reference Intervals Blood Component Reference Interval Hemoglobin (altitude dependent) Male adult 14-18 g/ dL (140-180 mmol/ L) Female adult 12-16 g/ dL (120-160 mmol/ L) Hematocrit (altitude dependent) Male adult 42%-52% (0.42-0) Female adult 37%-47% (0.37-0)
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 117
- Fasting blood glucose levels are used to help diagn ose diabetes m ellitus and hypoglycem ia.
- Instruct the client to fast for 8 to 12 hours before the test.
- Instruct a client with diabetes m ellitus to with- hold m orning insulin or oral hypoglycem ic m ed- ication until after the blood is drawn.
- Norm al reference interval: glucose (fasting) 70-110 m g/dL (4-6 m m ol/L)
J. Glycosylated hem oglobin (HgbA1C)
HgbA1C is blood glucose bound to hem oglobin.
Hem oglobin A1c (glycosylated hem oglobin A; HbA1c) is a reflection of how well blood glucose levels have been controlled for the past 3 to 4 m onth s.
Hyperglycem ia in clients with diabetes is usually a cause of an increase in the HbA1c.
Fasting is not required before the test.
Norm al reference intervals: 4%–6% (4%– 6%)
HgbA1C and estim ated average glucose (eAG) reference intervals (Table 10-4).
K. Renal function studies
- Serum creatinine a. Creatinine is a specific indicator of renal function. b. Increased levels of creatinine indicate a slow- ing of the glom erular filtration rate. c. Instruct the client to avoid excessive exercise for 8 hours and excessive red m eat intake for 24 hours before the test. d. Norm al reference interval: 0–1 m g/dL (53–115 μm ol/L)
- Blood urea nitrogen (BUN) a. Urea nitrogen is the nitrogen portion of urea, a substance form ed in the liver through an enzym atic protein breakdown process. b. Urea is norm ally freely filtered through the renal glom eruli, with a sm all am ount reab- sorbed in the tubules and the rem ainder excreted in the urine. c. Elevated levels indicate a slowing of the glo- m erular filtration rate. d. BUN and creatinine ratios should be analyzed when renal function is evaluated. e. Norm al reference interval: 6–20 m g/dL (2– 7 m m ol/L)
L. White blood cell (WBC) count
- WBCs function in the im m un e defense system of the body.
- The WBC differen tial provides specific inform a- tion on WBC types.
- A “shift to the left” (in the differential) m eans that an increased num ber of im m ature neutro- phils is present in the blood.
- A low total WBC count with a left shift indicates a recovery from bone m arrow depression or an infec- tion of such intensity that the demand for neutro- phils in the tissue is higher than the capacity of the bone m arrow to release them into the circulation.
- A high total WBC coun t with a left shift indicates an increased release of neutrophils by the bone m arrow in response to an overwh elm in g infec- tion or inflam m ation.
- An increased neutrophil coun t with a left shift is usually associated with bacterial infection.
- A “sh ift to the right” m eans that cells have m ore than the usual num ber of nuclear segm ents; found in liver disease, Down syndrom e, and m egaloblastic and pernicious anem ia.
- Norm al reference interval: 5000–10,000 m m 3 (5–10 Â 10 9 /L)
Monitor the WBC count and differential closely in cli- ents receiving chemotherapy because of the risk for neu- tropenia; neutropenia places the client at risk for infection.
TABLE 10-3 Lipids: Reference Intervals Blood Component Reference Interval Cholesterol < 200 mg/ dL (< 5 mmol/ L) High-density lipoproteins (HDLs)
Male: > 40 mg/ dL (> 1 mmol/ L) Female: > 50 mg/ dL (> 1 mmol/ L)
Low-density lipoproteins (LDLs)
Recommended: < 100 mg/ dL (< 2 mmol/ L) Near optimal: 100-129 mg/ dL (2.6-3 mmol/ L) Moderate risk for coronary artery disease (CAD): 130-159 mg/ dL (3.37-4 mmol/ L) High risk for CAD: > 160 mg/ dL (> 4 mmol/ L) Triglycerides < 150 mg/ dL (< 1 mmol/ L)
TABLE 10-4 Glycosylated Hemoglobin (HgbA1C) and Estimated Average Glucose (eAG) HgbA1C % eAG mg/ dL eAG mmol/ L 6 126 7. 6 140 7. 7 154 8. 7 169 9. 8 183 10. 8 197 10. 9 212 11. 9 226 12. 10 240 13.
American Diabetes Association, DiabetesPro: Estimated average glucose, eAG/ A1C Conversion Calculator (website): http:/ /professional.diabetes/ diapro/ glucose_calc.
118 UNIT III Nursing Sciences
70. The nurse is caring for a client who takes ibuprofen
for pain. The nurse is gathering inform ation on the client’s m edication history, and determ ines it is nec- essary to contact the health care provider (HCP) if the client is also taking which m edications? Select all th at apply. 1. Warfarin 2. Glim epiride 3. Am lodipine 4. Sim vastatin 5. Hydrochlorothiazide
71. A client with diabetes m ellitus has a glycosylated
hem oglobin A1c level of 9%. On the basis of this test result, the nurse plans to teach the client about the need for which m easure?
- Avoiding infection
- Taking in adequate fluids
- Preventing and recognizing hypoglycem ia
- Preven ting and recognizing hyperglycem ia
72. The nurse is caring for a client with a diagn osis of
cancer who is im m unosuppressed. The nurse would consider im plem enting neutropenic precautions if the client’s white blood cell count was which value?
- 2000 m m 3 (2 Â 10 9 /L)
- 5800 m m 3 (5 Â 10 9 /L)
- 8400 m m 3 (8 Â 10 9 / L)
- 11,500 m m 3 (11 Â 10 9 /L)
73. A client brought to the em ergency departm en t states
that he has accidentally been taking 2 tim es his pre- scribed dose of warfarin for the past week. After not- ing that the client has no evidence of obvious bleeding, the nurse plans to take which action?
Prepare to adm inister an antidote.
Draw a sam ple for type and crossm atch and transfuse the client.
Draw a sam ple for an activated partial throm bo- plastin tim e (aPTT) level.
Draw a sam ple for prothrom bin tim e (PT) and international norm alized ratio (INR).
74. The nurse is caring for a postoperative client who is
receiving dem and-dose hydrom orph one via a patien t-con trolled analgesia (PCA) pum p for pain control. The nurse enters the clien t’s room and finds the client drowsy and records the following vital signs: tem perature 97 °F (36 °C) orally, pulse 52 beats per m inute, blood pressure 101/ 58 m m Hg, respiratory rate 11 breath s per m inute, and SpO 2 of 93% on 3 liters of oxygen via nasal cann ula. Which action should the nurse take n ext?
- Docum ent the findin gs.
- Attem pt to arouse the client.
- Contact the health care provider (HCP) im m ediately.
- Check the m edication adm inistration history on the PCA pum p.
75. An adult fem ale clien t has a hem oglobin level of
10 g/dL (108 m m ol/L). The nurse interprets that this result is m ost likely caused by which condition noted in the clien t’s history?
- Dehydration
- Heart failure
- Iron deficiency anem ia
- Chronic obstructive pulm onary disease
76. A client with a history of gastrointestinal bleeding
has a platelet count of 300,000 m m 3 (300 Â 10 9 /L). The nurse should take which action after seeing the laboratory results?
- Report the abnorm ally low count.
- Report the abnorm ally high count.
- Place the clien t on bleeding precautions.
- Place the norm al report in the client’s m edical record.
A N S W E R S
63. 2
Ra tiona le: The norm al PT is 11 to 12 seconds (conventional therapy and SI units). The norm al INR is 2 to 3 for standard warfarin therapy, which is used for the treatm ent of atrial fibril- lation, and 3 to 4 for high-dose warfarin therapy, which is used for clients with m echanical heart valves. A therapeutic PT level is 1 to 2 tim es higher than the norm al level. Because the values of 35 seconds and 3 are high, the nurse should anticipate that the client would not receive further doses at this tim e. Therefore, the prescriptions noted in the rem aining options are incorrect. Test-Ta king Stra tegy: Focus on the su b ject , a PT of 35 seconds and an INR of 3. Recall the norm al ranges for these values
and rem em ber that a PT greater than 32 seconds and an INR greater than 3 for standard warfarin therapy places the client at risk for bleeding; this will direct you to the correct option. Review: The n o r m al p r o th r o m b in tim e an d INR levels Level of Cognitive Ability: Analyzing Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Analysis Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Clotting References: Lewis et al. (2014), p. 627; Rosenjack Burchum , Rosenthal (2016), pp. 622–623.
64. 4
Ra tiona le: Pain is a highly individual experience, and the new graduate nurse should not assum e that the client is
120 UNIT III Nursing Sciences
exaggerating his pain. Rather, the nurse should frequently assess the pain and intervene accordingly through the use of both nonpharm acological and pharm acological interventions. The nurse should assess pain using a num ber-based scale or a picture-based scale for clients who cannot verbally describe their pain to rate the degree of pain. The nurse should follow up with the client after giving m edication to ensure that the m edication is effective in m anaging the pain. Pain experienced by the older client m ay be m anifested differently than pain experienced by m em bers of other age groups, and they m ay have sleep disturbances, changes in gait and m obility, decreased socialization, and depression; the nurse should be aware of this attribute in this population. Test-Taking Strategy: Note the str at egic wor ds, need for further teaching. These words indicate a n egative even t query and the need to select the incorrect statement as the answer. Recall that pain is a highly individual experience, and the nurse should not assume that the client is exaggerating pain. Review: Man agem en t o f p ain Level of Cognitive Ability: Evaluating Client Needs: Physiological Integrity Integra ted Process: Teaching and Learning Content Area : Fundam entals of Care—Pain Priority Concepts: Clinical Judgm ent; Pain Reference: Lewis et al. (2014), pp. 122, 134.
65. 2
Ra tiona le: The norm al BUN level is 6 to 20 m g/dL (2 to 7 m m ol/L). Values of 29 m g/dL (10 m m ol/L) and 35 m g/dL (12 m m ol/L) reflect continued dehydration. A value of 3 m g/ dL (1 m m ol/ L) reflects a lower than norm al value, which m ay occur with fluid volum e overload, am ong other conditions. Test-Ta king Stra tegy: Focus on the su b ject , adequate fluid replacem ent and the norm al BUN level. The correct option is the only option that identifies a norm al value. Review: The norm al b lo o d u r ea n itr o gen level Level of Cognitive Ability: Evaluating Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Evaluation Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Fluid and Electrolyte Balance References: Lewis et al. (2014), p. 1057; Pagana, Pagana (2014), pp. 511–514.
66. 2
Ra tiona le: An oral tem perature should be avoided if the client has nasal congestion. One of the other m ethods of m easuring the tem perature should be used according to the equipm ent available. Taking a rectal tem perature for a client who has under- gone nasal surgery is appropriate. Other, less invasive m easures should be used if available; if not available, a rectal tem perature is acceptable. Taking an axillary tem perature on a client who just consum ed coffee is also acceptable; however, the axillary m ethod of m easurem ent is the least reliable, and other m ethods should be used if available. If tem poral equipm ent is available and the client is diaphoretic, it is acceptable to m ea- sure the tem perature on the neck behind the ear, avoiding the forehead.
Test-Ta king Stra tegy: Note the st r ategic wo r d s, need for fur- ther teaching. These words indicate a n egative even t qu er y and the need to select the incorrect action as the answer. Recall that nasal congestion is a reason to avoid taking an oral tem - perature, as the nasal congestion will cause problem s with breathing while the tem perature is being taken. Review: Tem p er atu r e m easu r em en t m eth o d s Level of Cognitive Ability: Evaluating Client Needs: Safe and Effective Care Environm ent Integra ted Process: Teaching and Learning Content Area : Fundam entals of Care—Vital Signs Priority Concepts: Teaching and Learning; Therm oregulation Reference: Perry, Potter, Ostendorf (2014), pp. 68–69, 76.
67. 4
Ra tiona le: The norm al aPTT varies between 28 and 35 seconds (28 and 35 seconds), depending on the type of activator used in testing. The therapeutic dose of heparin for treatm ent of deep vein throm bosis is to keep the aPTT between 1 (42 to 52) and 2 (70 to 87) tim es norm al. This m eans that the client’s value should not be less than 42 seconds or greater than 87 seconds. Thus the client’s aPTT is within the therapeutic range and the dose should rem ain unchanged. Test-Taking Strategy: Focus on th e su b ject, th e expected aPTT for a clien t receivin g a h eparin sodium in fusion. Rem em ber th at th e norm al ran ge is 28 to 35 secon ds an d th at th e aPTT sh ould be between 1 an d 2 tim es n orm al wh en th e clien t is receivin g h eparin th erapy. Sim ple m ultiplication of 1 an d 2 by 28 an d 35 will yield a ran ge of 42 to 87 secon ds). Th is clien t’s value is 65 secon ds Review: The aPTT level and the expected level if the client is receiving h ep ar in Level of Cognitive Ability: Analyzing Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Analysis Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Clotting Reference: Lewis et al. (2014), p. 627.
68. 1
Ra tiona le: The norm al serum potassium level in the adult is 3 to 5 m Eq/L (3 to 5 m m ol/ L). The correct option is the only value that falls below the therapeutic range. Adm inis- tering furosem ide to a client with a low potassium level and a history of cardiac problem s could precipitate ventricular dys- rhythm ias. The rem aining options are within the norm al range. Test-Ta king Stra tegy: Note th e su b ject of th e question , th e level th at sh ould be reported. Th is in dicates th at you are lookin g for an abn orm al level. Rem em ber, th e n orm al serum potassium level in th e adult is 3 to 5 m Eq/ L (3 to 5 m m ol/ L). Th is will direct you to th e correct option. Review: The norm al ser u m p o tassiu m level Level of Cognitive Ability: Applying Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Im plem entation Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Fluid and Electrolyte Balance
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 121
Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Planning Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Clotting Reference: Lewis et al. (2014), p. 627.
74. 2
Ra tiona le: The prim ary concern with opioid analgesics is respi- ratory depression and hypotension. Based on the assessm ent findings, the nurse should suspect opioid overdose. The nurse should first attem pt to arouse the client and then reassess the vital signs. The vital signs m ay begin to norm alize once the cli- ent is aroused because sleep can also cause decreased heart rate, blood pressure, respiratory rate, and oxygen saturation. The nurse should also check to see how m uch m edication has been taken via the PCA pum p, and should continue to m onitor the client closely to determ ine if further action is needed. The nurse should contact the HCP and docum ent the findings after all data are collected, after the client is stabilized, and if an abnor- m ality still exists after arousing the client. Test-Ta king Stra tegy: First, note the str ategic wo r d , next. Fo cu s o n th e d ata in t h e qu estio n and d eter m in e if an ab n o r m ality exists. It is clear that an abnorm ality exists because the client is drowsy and the vital signs are outside of the norm al range. Recall that attem pting to arouse the client should com e before further assessm ent of the pum p. The client should always be assessed before the equipm ent, before con- tacting the HCP, and before docum entation. Review: Managem ent of potential o p io id o ver d o se. Level of Cognitive Ability: Synthesizing Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Im plem entation Content Area : Fundam entals of Care—Pain Priority Concepts: Clinical Judgm ent; Pain Reference: Lewis et al. (2014), p. 164.
75. 3
Ra tiona le: The norm al hem oglobin level for an adult fem ale client is 12–16 g/dL (120–160 m m ol/L). Iron deficiency
anem ia can result in lower hem oglobin levels. Dehydration m ay increase the hem oglobin level by hem oconcentration. Heart failure and chronic obstructive pulm onary disease m ay increase the hem oglobin level as a result of the body’s need for m ore oxygen-carrying capacity. Test-Ta king Stra tegy: Note the str at egic wo r d s, most likely. Evaluate each of the conditions in the options in term s of their pathophysiology and whether each is likely to raise or lower the hem oglobin level. Also, note the relationship between hem oglobin level in the question and the correct option. Review: The norm al h em o glo b in level Level of Cognitive Ability: Analyzing Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Assessm ent Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Gas Exchange Reference: Lewis et al. (2014), pp. 628, 638.
76. 4
Ra tiona le: A norm al platelet count ranges from 150,000 to 400,000 m m 3 (150 to 400 Â 10 9 /L). The nurse should place the report containing the norm al laboratory value in the client’s m edical record. A platelet count of 300,000 m m 3 (300 Â 10 9 /L) is not an elevated count. The count also is not low; therefore, bleeding precautions are not needed. Test-Ta king Stra tegy: Focus on the su b ject , a platelet count of 300,000 m m 3 (300 Â 10 9 /L). Rem em ber that options that are co m p ar ab le o r alike are not likely to be correct. With this in m ind, elim inate options indicating to report the abnorm ally low count and placing the client on bleeding precautions first. From the rem aining options, recalling the norm al range for this laboratory test will direct you to the correct option. Review: The norm al p latelet co u n t Level of Cognitive Ability: Applying Client Needs: Physiological Integrity Integra ted Process: Nursing Process—Im plem entation Content Area : Fundam entals of Care—Laboratory Values Priority Concepts: Clinical Judgm ent; Clotting Reference: Lewis et al. (2014), p. 626.
CHAPTER 10 Vital Signs and Laboratory Reference Intervals 123
Saunders Vital Signs and Laboratory Reference Intervals RN Nclex
Course: Adult Health II (NUR 2211)
University: Hillsborough Community College

- Discover more from:
Recommended for you
Students also viewed
- Saunders Parenteral Nutrition RN Nclex
- Saunders Acid-Base Balance RN Nclex
- Saunders Ch. 6 Ethical and Legal Issues RN Nclex
- Saunders 7th Edition Integumentary Disorders of the Adult Client : Integumentary System RN Nclex
- Saunders Psychiatric Medications RN Nclex 68
- Saunders Foundations of Mental Health Nursing RN Nclex 64