- Information
- AI Chat
Week 1 Pharmacology
Nursing Pharmacology
Keiser University
Recommended for you
Related Studylists
PharmacologyPreview text
Week 1 Pharmacology
Introduction to Nursing Pharmacology
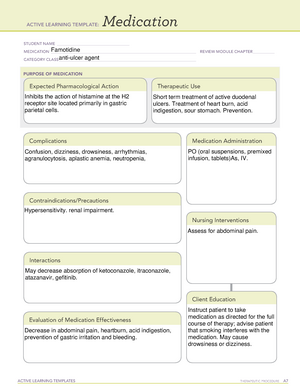
Therapeutic and Pharmacologic Classifications
o Describes what is being treated o Drugs are placed into a therapeutic class based on the usefulness in treating a specific disease “Anti-“ often refers to a therapeutic class o Addresses a drug’s mechanism of action or how the drug produces its effect in the body. o A drug’s pharmacologic classification is more specific than its therapeutic classification and requires an understanding of biochemistry and physiology. o Understanding the mechanism of action of a drug will help you anticipate what to watch for in your patient.
Naming Drugs
o Chemical Name o Generic Name o Brand Name
Controlled Substances
o Drugs with potential for abuse are categorized into 5 DEA schedules o Use is restricted and highly regulated
Generic Drugs
o Chemicals produced by companies involved solely in the manufacturing of drugs.
o Cheaper o Binders used in generic drugs may not be the same as those in brand name drugs. o The bioavailability of a generic drug may be different from the brand name drug o Many states require that a drug be dispensed in the generic form if available o If prescription states, “Dispensed as written” (DAW), then the brand name drug must be used.
Orphan Drugs
o Treating rare diseases o Potentially dangerous adverse effects o Often abandoned after preclinical trials or phase 1 studies o Orphan Drug Act of 1983
Over the Counter (OTC) Drugs
o No prescription needed o Cheaper o Choosing the proper medication for a specific problem can be challenging o Drug interactions with food, herbal supplements, prescription drugs or other OTC drugs. o Common for patients to not report using OTC drugs o Self-treatment is sometimes ineffective o Mask signs and symptoms of an underlying disease.
Drug Labels and Package Inserts
o Labels have specific information
o Chemotherapy destroys both normal and abnormal cells (results are many of the adverse effects associated with these drugs) These drugs affect cells that reproduce or are replaced rapidly are more easily affected by these drugs (bone marrow, GI cells, hair follicles) o Dosing of chemotherapy is most important to kill invading cells and cause the least amount of toxicity to the host.
Pharmacokinetics
o How the body acts on a drug after administration o Focus is on ADME (Absorption, Distribution, Metabolism, and Excretion) o Critical concentration, loading dose, and dynamic equilibrium Loading Dose: higher than the standard dose for a more rapid response. Critical concentration: recommended dose Dynamic equilibrium: a state of balance between continuing processes.
Absorption
o Movement of a drug from site of administration to the bloodstream o Route of administration IM, subcu, oral, rectal, dermal o Factors that affect absorption o Absorption processes: Filtration = drug excretion Passive diffusion: from higher to lower concentration. Active transport: moving against concentration gradient
Distribution
o Involves the movement of a drug into the body’s tissues o Factors affecting distribution: Blood flow (perfusion of the reactive tissue) Drugs lipid solubility Protein binding Blood-brain barrier Placenta and breast milk
Biotransformation (Metabolism)
o Processes that change the activity of a drug and make it more likely to be excreted o Most important site for metabolism: Liver o Factors affecting metabolism: First-pass effect Absorbed in stomach – metabolized in liver. Hepatic enzymes Aid in metabolism of drugs that are harder to breakdown, increases risk of toxicity.
Excretion
o Removal of a drug from the body o Filtration (glomerular filtration) o Important organ for excretion: Kidneys Important to know patients kidney function. o Other routes used to excrete drugs: Skin, Lungs, Saliva, Feces, Bile (hepatic).
Time-response Relationships
o Primary actions – exaggerated therapeutic effect. (blood thinner = too much blood loss). o Secondary actions – Side effects already documented in literature (everything has side effects but this would be intolerable). o Hypersensitivity reactions – excessive response (allergic reactions, severe reactions).
Drug Allergy
o Occurs when the body forms antibodies to a particular drug Can only occur if patient has been exposed to the drug before. o Cross allergies (cross-sensitivities) o Four classifications Anaphylactic reactions Cytotoxic reactions – attack antigens of a specific drug causing cell death. (Checked through blood work) Serum sickness – the already circulating antibodies cause damage to actual tissue. (Rash, high fever, join pain). Occurs in patients who have taken the drug before. Delayed reactions
Drug-Induced Tissue and Organ Damage
o Dermatological Reactions Simple to fatal Hives, rash, lesions scaly, fever, lymphadenopathy. Does the benefit of the drug outweigh the discomfort? Severe cases – discontinue. o Stomatitis
Inflammation of the mucous membranes Swollen hums, gingivitis, glossitis, dysphagia, bad breath Frequent mouth care: nutrition eval; small, frequent meals; dental consult.
o Superinfections
Infections caused by organisms that are usually controlled by the normal flora Fever, diarrhea, black or hairy tongue, glossitis, mucitis. Supportive measures
o Blood dyscrasia
Bone marrow suppression caused by drug effects when drugs cause cell death Fever, chills, sore throat, weakness, back pain, dark urine, low WBC, decreased HCT, thrombocytopenia Monitor blook counts; supportive measures; if severe, discontinue drug totally or until bone marrow recovers.
o Liver Injury
Affected by first-pass effect, exposing liver to full impact of the drug before breakdown. Fever, malaise, nausea, vomiting, jaundice, change in color or urine or stools, abdominal pain, elevated liver enzymes, bilirubin, and clotting factors. Discontinue drug, supportive measures
o Renal Injury
Occurs when drug molecules plug the capillary network of the glomerulus
Replace potassium, cardiac monitoring. o Hyperkalemia High serum potassium levels >5 mEq/L Weakness, muscle cramps, diarrhea, numbness and tingling, bradycardia, hypotension, decreased urine output, difficulty breathing Sodium polystyrene sulfonate decreases serum potassium concentration, cardiac monitoring
Sensory Effects
o Ocular Damage Occurs when drugs are deposited into the tiny blood vessels in the retina, causing inflammation and tissue damage. Blurred vision, color vision changes, corneal damage, blindness Monitor vision when patient is receiving oculotoxic drugs, monitor lighting and exposure to sunlight o Auditory Damage Occurs when the tiny vessels and nerves in CN VIII are irritated and damaged Dizziness, tinnitus, loss of balance, loss of hearing Monitor patient’s perceptual losses or changes, safety precautions, may need dose decreased or discontinued.
Neurological Effects
o General CNS Effects Occurs when blood-brain barrier is broken Confusion, delirium, insomnia, drowsiness, hallucinations, tingling, paresthesia
Safety measures, educate to avoid dangerous situations, dose may be decreased or discontinued o Atropine-Like (Anticholinergic) Effects Occurs when a drug block the effects of the parasympathetic nervous system by directly or indirectly blocking cholinergic receptors Dry mouth, altered taste, constipation, paralytic ileus, urinary hesitancy and retention, nasal congestion, palpitations, tachycardia. Supportive measures o Parkinson-Like Syndrome Drugs that directly or indirectly affect dopamine levels in the brain can cause a syndrome that resembles Parkinson disease Lack of activity, muscular tremors, drooling, changes in gait, rigidity, extreme restlessness Discontinue drug (unless benefit outweighs the discomfort) o Neuroleptic Malignant Syndrome A syndrome caused by general anesthetics and drugs that have direct CNS effects High fever, slowed reflexes, rigidity, involuntary movements, HTN, tachycardia Discontinue drug
Teratogenicity
o Drugs that reach the developing fetus can cause death or congenital defects.
When in doubt, ask questions
Reporting Medication Errors
o Must be reported on national and institutional levels o Look-alike or sound-alike drug names o Common dosing errors o Transcribing issues o Always follow institutional policies for reporting errors o Reporting medication errors provides opportunities for education and helps identify areas where system changes may be needed.
Week 1 Pharmacology
Course: Nursing Pharmacology
University: Keiser University

- Discover more from:Nursing PharmacologyKeiser University651 Documents
- More from:Nursing PharmacologyKeiser University651 Documents