- Information
- AI Chat
Was this document helpful?
Module Three: Geriatric Care Models Lecture Notes
Course: Nursing Care of Older Adult (NUR 2214)
274 Documents
Students shared 274 documents in this course
University: Rasmussen University
Was this document helpful?

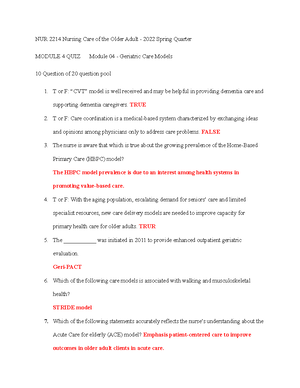
Module Four – Geriatric Care Models
Overview
Because of aging population, increased demand for health care, and limited resources
oNew care delivery models are initiated to improve capacity for primary health
care of older adults
oHelp to moderate healthcare costs and improve the patient’s experience
oFocus on health promotion and disease prevention
Access barriers to social support and/or financial resources can lead to missed
appointments, fragmented care, and poor control of chronic conditions
The purpose of most care models in older adults is to target interventions to maintain
health and well-being
Acute Care for Elderly (ACE)
Continuous quality improvement model
Emphasis patient-centered care to improve outcomes in older adult clients in acute care
How does it work?
oFrequent (daily) team meetings/rounds
Clearly defined structure and goals for the rounds
Requires training
oMethod of communicating team recommendations
Will patient’s physicians attend the rounds?
Many units use informal communication sheets
oOngoing geriatric and team functioning training
Interdisciplinary team care in hospitalized older adults
oReduced mortality
oImproved functional performance
oMore likely to be living at home after discharge
oReduced use of restraints
oReduced use of inappropriate medications
oReduced delirium
oReduced length of stay
oReduced health care utilization costs
oImproved patient and provider satisfaction
Healthy Aging Brain Center (HABC)
Developed to support primary care providers in the specialized diagnosis and
management of patients with cognitive impairment caused by conditions such as
Alzheimer’s, delirium, and cognitive and emotional problems that may arise after critical
illnesses
Working closely with the patient’s primary care provider, the multidisciplinary care team
oPhysicians
oNurses
oPsychologists
oSocial workers
Students also viewed
Related documents
- Nursing of older adults
- 2024 Nclex RN Test Bank with NGN 150 New Generation NGN Questions & Answers,latest version && 100% Verified Actual Exam Questions & Answers Rationales Compilations 2024
- 2024 Nclex RN Test Bank with NGN 150 New Generation NGN Questions & Answers,latest version && 100% Verified Actual Exam Questions & Answers Rationales Compilations 2024#
- 2024 Nclex RN Test Bank with NGN 150 New Generation NGN Questions & Answers,latest version &&100% Verified Actual Exam Questions & Answers Rationales Compilations 2024,,#&#
- 2024 RN ATI Adult Medical Surgical Proctored Exam 2024 With 70 NGN Questions And Answers & Rationales,&&& 100% %Verified Actual Exam Questions & Answer Compilations 2024
- Care Plan for Older Adults