- Information
- AI Chat
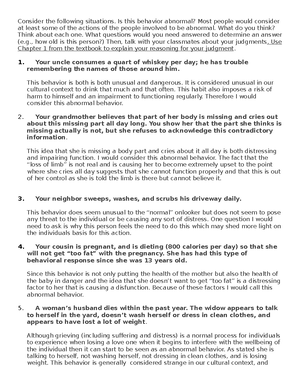
Abnormal psyc cummulative section of the final
Abnormal Psychology (PSYC 3303)
University of Colorado Boulder
Preview text
Abnormal Psych Study Guide
Cumulative Section of the Final Exam
Fall 2022
Note: This guide is only for the cumulative section, which is the majority of the final exam. Topics discussed following Exam 3 (Eating Disorders, Schizophrenia, and Personality Disorders) will be on the final but are not included in this guide.
Only Perusall 7 (The concept of schizophrenia) will be on the final exam.
Be able to define, recognize, or provide examples for the following terms: (on Quizlet) quizlet/750893869/abnormal-psych-final-flash-cards/
Here’s another helpful quizlet I found! Good luck on the exam you got this :) quizlet/585638839/abnormal-3-flash-cards/
Incidence Prevalence Prodromal A course of a disorder (chronic, episodic) Prognosis Etiology Multidimensional integrative approach Anosognosia Diathesis-Stress Model Behavioral Model Operant Conditioning
- Positive reinforcement
- Negative reinforcement Classical Conditioning Modeling (Observational Learning) Cognitive Science Equifinality Multifinality Diagnosis Prototypical approach Comorbidity Analogue Study Case study Correlations (positive, negative)
Randomized Clinical Trial Statistical vs Clinical significance Placebo Effect Nocebo Effect Fear Anxiety Agoraphobia Anxiety sensitivity Interoceptive awareness Double depression Depression with melancholic vs. atypical features
Be prepared to answer questions about: Criticisms of the DSM- ➢ Critics of the medicalization of normality ➢ Increased number of diagnoses ➢ Lowered thresholds of conditions If ‘anxiety’ is an emotion we can expect to experience – what makes anxiety disorders different from anxiety? Experiencing occasional anxiety is a normal part of life. However, people with anxiety disorders frequently have intense, excessive, and persistent worry and fear about everyday situations. If avoidance is what maintains a disorder then what is likely a key component of treatment? Exposure to the problem and fear is worsening the disorder. Such as exposure treatment for phobias or not letting someone with OCD complete a ritual in order for them to face their intrusive thoughts. Panic attack/panic disorder: symptoms, etiology, and treatment ⭐Important note: you can have a panic attack without having a panic disorder Symptoms of a panic attack 11 somatic symptoms: ➢ Increased heart rate ➢ Shortness of breath ➢ Chest pain ➢ Choking sensation ➢ Trembling ➢ Sweating ➢ Nausea ➢ Dizziness ➢ Numbness ➢ Hot flashes or chills
Hypervigilance to symptoms, interoceptive awareness, anticipatory anxiety, and memory of past attacks Increased anxiety and fear Panic control treatment ➢ Step 1: Psychoeducation ➢ Step 2: Generate multiple interpretations of bodily sensations ➢ Step 3: Tools to cope with anxiety ➢ Step 4: Interoceptive exposure (exposure therapy): Rationale which is where you provide opportunities to examine negative predictions about internal sensations and increase tolerance to and acceptance of internal sensations. The second is the method: engage in systematic exercises that induce feared internal sensations (dizziness, heart rate) CBT decreases avoidance, fear of phobic situations, and anxiety symptoms based on self-report scales What is the difference between being afraid of something and having a diagnosable phobia? What makes something a phobia is an obsession over the phobia and most of the time it is unreasonable or excessive. People with phobias will go to great lengths to avoid what their phobia is if someone has a phobia of spiders, they’ll avoid basements and refuse to go to them. It occupies their mind a lot more than just a regular fear does. Remember the story of the professor’s client who bought new luggage to avoid going down to the basement to grab their luggage because of their spider phobia. Phobia diagnosis/treatment - how is Blood-Injection-Injury Phobia different from other phobias? Phobia DSM checklist: 1. Marked, disproportionate and persistent fear of anxiety about one or more social situations where they are exposed to possible scrutiny 2. Fear of being negatively evaluated by or offensive to others 3. Anxiety is almost always produced by exposure to social situations 4. Avoidance of feared situations 5. Significant distress or impairment Treatment: Almost always exposure-based Systematic desensitization ➢ Teach relaxation skills ➢ Create fear hierarchy (stimulus hierarchy) ➢ Pair relaxation with the feared objects or situations ➢ Since relaxation is incompatible with fear, the relaxation response is thought to substitute for the fear response ➢ 1-5 sessions Other behavioral treatments: Flooding
- Nongradual exposure Modeling
- The therapist confronts the feared object while the fearful person observes The key to success is actual contact with the feared object or situation
Blood phobias: Different from other phobias because it can cause the person to pass out or faint when receiving or giving blood. It also causes the person to avoid going to the doctor or receiving medical help. Blood-injection-injury type: Medical procedures or observing blood ➢ Each year, 8% of all people in the U have symptoms of a specific phobia ➢ Many suffer more than one phobia at a time ➢ Women outnumber men 2: ➢ The vast majority of people with a specific phobia do not seek treatment Social Anxiety Disorder – diagnosis and behavioral/cognitive factors Severe, persistent, and unreasonable fears of social or performance situations in which embarrassment may occur - Performance only: talking, performing, eating or writing in public - Broad: General fear of functioning poorly in front of others DSM-5 Checklist 1. Marked, disproportionate and persistent fear of anxiety about one or more social situations where they are exposed to possible scrutiny 2. Fear of being negatively evaluated by or offensive to others 3. Anxiety is almost always produced by exposure to the social situation 4. Avoidance of feared situations 5. Significant distress of impairment They believe that - They are socially unskilled and inadequate - They are always in danger of behaving incompetently in social situations - Inept behaviors in social situations will inevitably lead to terrible consequences Can greatly interfere with one's life (often kept a secret) - 7% of people in the U experience a social anxiety disorder in any given year - Women outnumber men 3: - Phobias often begin in childhood and may persist for many years Cognitive Traps - "Everyone else looks so much more relaxed" "What if I say something dumb" - These thoughts start to rapidly spiral out of control to the point that anything anyone else has said is missed. People may say as little as possible and hope that no one has noticed their anxiety - Negative beliefs: Strongly held beliefs about inadequacy in social and/or performance-related situations
➢ Addresses cognitive issues that contribute to hyperarousal such as worrying about sleep, excessive monitoring, and sleep effort ➢ Outperforms medications in the long-term positive effects of CBT-I were still present after 10 years post-treatment. Insomnia severity remained low and two-thirds of participants no longer fulfilled the criteria for an insomnia diagnosis. Medication ➢ Ambien ➢ Lunesta ➢ Belsomra ➢ Sedating antidepressants (Trazadone) ➢ Cannabis ➢ Melatonin What are obsessions and compulsions and how are they related? Obsessions:
- Recurrent and persistent thoughts urge, or impulses that are experienced at some time during the disturbance, as intrusive and unwanted and that in most individuals cause marked anxiety or distress
- The individual attempts to ignore or suppress such thoughts urges or images, or to neutralize them with some other thought or action Compulsions
- Repetitive behaviors or mental acts that the individuals feel driven to perform in response to an obsession or according to rules that must be applied rigidly
- The behaviors or mental acts are aimed at preventing or reducing anxiety or distress or preventing some dreaded event or situation. The obsessions or compulsions are time-consuming or cause clinically significant distress or impairment What are the event characteristics and vulnerability factors associated with PTSD? Event characteristics/stressors from DSM5: ➢ Exposed to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence: Direct exposure, witnessing (in person), indirectly by learning that a close relative or close friend was exposed to trauma ➢ Repeated or extreme indirect exposure to aversive details of the events, usually in the course of professional duties (first responders, collecting body parts, exposure to child abuse) This does not include indirect non-professional exposure. Vulnerability factors: Event characteristics:
- Severity
- Duration
- Proximity
- Human-generated stressors
Social influences - Social support reduces the intensity of physical and emotional triggers or stress. Lack of social support intensifies symptoms. Prime strategies for treating OCD, PTSD, and other anxiety disorders. All of the possible treatments include SSRIs. Treatment for OCD: ➢ Exposure to situations that elicit obsessions ➢ Exposes person to the full force of anxiety ➢ Prevention from engaging in compulsive behaviors ➢ Promotes extinction of conditioned response ➢ Exposure hierarchy begins with tackling less threatening stimuli and progresses to more threatening stimuli ➢ 69-75% show significant improvement ➢ Among people with OCD, 1/3 unwilling to begin ERP Treatment for PTSD: Cognitive Processing Therapy (CPT) ➢ Cognitive therapy and exposure in the form of writing and reading about the traumatic event ➢ Erroneous beliefs about cause and consequences ➢ Initial focus on self-blame and then overgeneralized beliefs about oneself and the world. Goals of exposure therapies: ➢ Extinguish fear response ➢ Promote mastery by providing experiences of coping with memories and PTSD symptoms Medications ➢ SSRIs because they decrease hyperarousal and mood. Somewhat less effective for the symptoms of reexperiencing ➢ Prazosin (for nightmares) ➢ Service dogs, trained tasks include picking up cues of distress or anxiety and consequently nudging, pawing or licking them to encourage the veteran to focus on the dog. ➢ Also trained to notice when veterans are experiencing anxiety and will actively wake up the person from nightmares. Someone has experienced a traumatic event: what is the biggest protective factor that could prevent the development of PTSD? What are examples of risk factors for developing PTSD after a traumatic event? The biggest protector factor for developing PTSD is social support. PTSD with Delayed Expression (why does this happen?) Full diagnosis is not met until at least six months after the trauma, although the onset of symptoms may occur immediately.
Depression, anxiety, memory, attention deficits, and significant social isolation.
Medications and psychotherapy for bipolar disorder Medications: ➢ Mood stabilizers: Lithium carbonate (first-line treatment), Lamotrigine, Cariprazine, and Valproic Acid ➢ Antidepressants ➢ Antipsychotics: Quetiapine (Seroquel), lurasidone (Latuda), Olanzapine (Zyprexa) Psychotherapy: ➢ Family-focused therapy helps understand vulnerability, learn the role of mood-stabilizing medications, reduce expressed emotions and distinguish between patient’s personality and their disorder. Substance Use Disorder symptoms/diagnosis
DSM5 Diagnosis: ➢ Alcohol use disorder, cocaine use disorder, nicotine use disorder, and opioid use disorder Substance-induced disorder: ➢ Alcohol intoxication, cocaine intoxication refers to a reversible set of symptoms occurring after use or exposure to a drug Alcohol withdrawal, nicotine withdrawal ➢ Diagnosed based on the behavioral, physical, and cognitive symptoms that occur due to the abrupt reduction or discontinuation of heavy and prolonged substance abuse Differences between Substance Use Disorder (addiction) vs being dependent on a medication Substance use disorder versus is based on withdrawal symptoms and the need to use large quantities of the substance to have an effect. Dependence is increased tolerance and withdrawal. Dependence is more severe. People who abuse a substance don’t make them addicted but they don’t necessarily have to have physical symptoms. The severity is substance use -> substance abuse ->substance dependence.
What is Narcan/naloxone and why is it important? Narcan is a life-saving medication you can give to someone who overdosed that will save their life by attaching to opioid receptors and reversing and blocking the effects of other opioids. What are the symptoms/issues related to different substance withdrawal syndromes? Symptoms of overdose (heroin, cocaine) Shallow breathing, confusion, lessened alertness, and loss of consciousness. Also, shallow breathing, confusion, lessened alertness, and loss of consciousness. How does craving play a role in the treatment of substance use disorders? Craving is a large factor in predicting relapse and the treatments help treat cravings and help people treat their thoughts/impulses when having cravings. How are substance use disorders treated: medications and psychotherapy Biological treatments: ➢ Agonist substitution: safer than drug abuse (methadone=opiate agonist, nicotine replacement) ➢ Antagonist: Block effect of drug abuse (naltrexone for heroin and alcohol) ➢ Partial agonist: Buprenorphine ➢ Aversive treatment: Disulfiram (Antabuse; alcohol) ➢ Vaccine: Theoretical basis: Sequester the drug in the blood via antibodies. Psychological treatments: ➢ CBT: What to do when the craving hits, activity planning, avoiding drug use, managing high-risk situations, refusal skills, and relapse prevention. ➢ AA/NA is 12 steps where you can avoid people/places/things. ➢ LifeRing: Sober self, group support, highlights, heartaches, plans for decision making
Great job working your way through this study guide!
Abnormal psyc cummulative section of the final
Course: Abnormal Psychology (PSYC 3303)
University: University of Colorado Boulder

- Discover more from: