- Information
- AI Chat
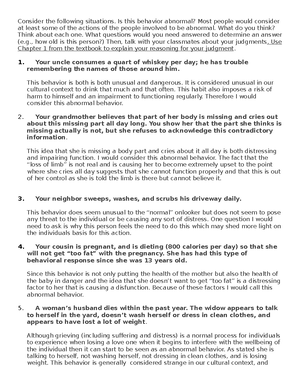
Abnormal Psych Study Guide for Exam 1
Abnormal Psychology (PSYC 3303)
University of Colorado Boulder
Preview text
Date of test: October 7th (Wednesday) @9am What’s covered? ★ Depression ★ Bipolar disorder ★ Panic disorder ★ Phobias ★ Social Anxiety disorder
Important definitions for mood disorders
Important factors for diagnosis: ➢ Intensity ➢ Duration ➢ Impairment in functioning ➢ Distress ➢ Mood patterns:
Euthymia: neutral mood A mood episode: Identified by a cluster of symptoms that occur together for a discrete period of time, and by the direction of the moods involved Mood disorder: Diagnoses are essentially defined by the patterns of mood disturbances observed through time
Major Depressive Disorder
In order for a diagnosis, there must be more than five of these symptoms present, most of the day (nearly every day) for more than two consecutive weeks: ● Depressed mood* ● Anhedonia (diminished ability to experience the pleasure that people typically enjoy)* ● Appetite disturbance ● Sleep disturbance ● Psychomotor agitation or retardation (are you moving or talking more quickly or slowly than usual) ● Fatigue ● Guilt/worthlessness ● Concentration problems or difficulty making decisions ● Suicidal thoughts
"Most recent episode" specifiers help with understanding prominent symptoms or etiology ● With psychotic features: delusions and hallucinations ● With seasonal pattern: seasonal affective disorder ● Atypical features (hypersomnia, increased appetite, and mood reactivity) ● Melancholic features (total anhedonia, circadian pattern, appetite or weight loss, guilt) ● Peripartum/Postpartum
Persistent Depressive Disorder (fewer symptoms for a longer duration) ● Depressed mood for most of the day, more days than not (2 years duration (not symptom-free more than 2 months)) along with more than two of the symptoms ● Accounts for o f22% of major depressive disorder (it can get worse than mild depression and is double depression) ● Longer treatment periods, higher doses of antidepressant medications ● Typical onset in the early 20s ● Earlier onset is associated with increased severity, duration, and heritability
Epidemiology of Major Depressive Disorder ● 8% of adults in the U suffer from severe unipolar depression in any given year (5% of women and 3% of men) ● An estimated 3% of the global population was affected, including 5% of adults and 5% of adults older than 60 ● Average onset=26 years old
Causes Biological causes Neurotransmitters: Serotonin and norepinephrine
● That avoidance makes depression worse and loss of opportunities to be positively reinforced through positive experiences Behavioral treatment: Behavioral activation: reintroduce people to pleasurable activities and events as well as concrete tasks and goals that reflect that patients' values, often using a weekly schedule. ● If you predict that you aren't going to enjoy something you usually do, you won't do it. ● When people start to do the things that they used to, it increases the brain's sensitivity to rewards Antidepressants: MAOIs, tricyclics, SSRIs,s and SNRIs ● The degree to which antidepressants suppress REM sleep has been associated with an overall enhanced antidepressant response Ketamine: ● The FDA approved ketamine nasal spray in conjunction with an oral antidepressant for the treatment of depression in adults who have tried other medications but haven't worked ● FDA's breakthrough therapy is a way of presenting a fast way to approval for drugs that display treatment advantages over current options for serious or life-threatening. ● 1 in 3 granted a breakthrough designation have ultimately moved to markets. Psilocybin: ● Breakthrough therapy designation was targeted for treatment-resistant depression. ● Depression diminished after 1 session and improvements were maintained at 1 month follow-up Electroconvulsive therapy (ECT) ● Very effective in the treatment of depression (60-80% of patients) ● Useful in people who have severe depression or delusions ● Mechanisms such as to why ECT works so well are being investigated ● Cognitive impairment tends to be transient and often resolves in the first few weeks after ECT
Bipolar Disorder
DSM5 Requirements (Requires changes in move and behavior that are extreme or uncharacteristic of the individual) The type of mood episodes determines the diagnosis Bipolar 1: You just need one manic episode and experiencing a major depressive episode isn't needed Bipolar 2: You need a hypomanic episode and a major depressive episode For a manic episode that needs 3 or more symptoms for a week: - Extreme elation or irritability and - Inflated self-esteem or grandiosity - Decreased need for sleep
- Rapid or pressured speech
- Racing thoughts or flight of ideas
- Excessive involvement in activities that have a high potential for painful consequences (engaging in spending sprees, foolish business investments)
- Increase in goal-directed activity
- Distractibility (attention too easily drawn to unimportant or irrelevant external stimuli) Hypomanic episode:
- A distinct periods of abnormality and persistently elevated, expanse, or irritable mood
- During the period of mood disturbance and increased energy or activity, more than 3 manic symptoms have persisted
- The mood usually isn't severe enough to cause significant problems with the person working
- The mood usually isn't severe enough to cause significant problems with the person working or socializing with others or to require hospitalization
- There are never any psychotic features present in a hypomanic episode
- The detection of hypomanic symptoms and longitudinal clinic assessment is crucial to differentiate a Biopolar disorder from other conditions (have to be able to detect another comorbid diagnosis) Bipolar with mixed features:
- The depressed episode with mixed features. Full criteria are met for depressive disorder and more than 3 hypomanic symptoms
- Manic or hypomanic episodes are mixed with features
- Mixed episodes are not pleasurable. Self-harm and suicide rates are higher in mixed states Prevalence: ● 1-3% lifetime prevalence ● BPi1=0.4-1% ● Late adolescence/early adulthood ● Rare after the age of 50 ● BP-1=18yo ● BP-2=Mid-20yo Sex differences: ● Females tend to have earlier onset and have a seasonal pattern ● Bipolar 2 is more likely to happen in females ● Rapid cycling: just having 4 depressed episodes in a year would qualify as rapid cycling even if the person never went above the line into mania or hypomania (more likely in females and having 4 or more is considered a lot) ● The same medication helps both sexes equally The course of bipolar disorder
Family Focused Therapy (usually with younger people) - Understanding vulnerability to future episodes - Learning the role of mood-stabilizing medications for symptom control - Reducing expressed emotion in communication - Making a difference between the personality and their disorder - Learning to cope with stressful events that can trigger episodes - Establishing functional relationships after a mood episode - After a 2 year follow-up, 52% did not relapse compared with 17% in the control group Interpersonal and Social Rythm Therapy - Address disruptions in or improve existing relationships (interpersonal relationships, employment stress, etc.) - Sensitivity to perturbations in circadian rhythm appears to be one major characteristic of bipolar disorders. Improve circadian rhythms through lifestyle regularity - Use of peripheral clocks (environmental signals to entrain circadian rhythm) such as meal times, exercise routines, screen time, and morning sunlight time.
Anxiety Disorders
The role of anxiety: ★ Increases preparedness ★ The absence of anxiety interferes with the performance ★ Moderate levels of anxiety improve performance ★ High levels of anxiety can be detrimental to performance ★ Anxiety is almost always cued ★ Misinterpretation of threat: overestimating the likelihood of negative outcomes and beliefs about the ability to cope What makes anxiety a disorder: ★ Severe enough to lower quality of life, chronic and frequent enough to interfere with functioning and out of proportion to the dangers involved Panic disorder: Important to know: you can have a panic attack without having a panic disorder Recurrent unexpected panic attacks Worry about feature panic attacks Worry about the consequences of the attack Substantial behavioral changes in response to the attacks Symptoms: - Increased heart rate - Shortness of breath - Chest pain - Choking sensation - Trembling
- Sweating
- Nausea
- Dizziness
- Numbness
- Hot flashes or chills
- Depersonalization or derealization 2 Cognitive symptoms
- Fear of dying
- Fear of losing control Biological factors:
- For heart attacks and they use EKG to measure the heart's electrical activity to see if you are actually having a heart attacks
- Atrial fibrillation which is also measured with EKG
- Doctors have to use an EKG when someone comes in with symptoms of a panic attack because they are so similar to heart attacks
- An increase in norepinephrine from the sympathetic nervous system increases the rate of contractions in the heart
- Along with adrenaline, norepinephrine also underlies the flight or fight response that increases the heart rate
- Misfiring or fight-flight system
- Parasympathetic nervous system not activated so fight-flight lingers. Brain Acidosis
- CO2 inhalation: breathing single or multiple breaths of co2 at concentrations from 5%-35% results in the accumulation of lactic acid in the brain
- One of the most consistent findings is that people with panic disorder have a panic attacks when doing the CO2 challenge
- People with panic disorder may be sensitive to lactic acid accumulating in acid-sensitive acid circuits Brain structure:
- Amygdala critical role in the circuits that control the experience of fear, both instinctive fear, and fear from life experiences. Maybe some hyperactivity of the amygdala
- The medial prefrontal cortex is the conscious processing of anxiety/fear: emotion regulation Prevalence:
- Around 2% of the U population is affected
- Females are twice as likely as males to be affected
- Cultural differences in types of symptoms of panic experienced Treatment:
- SSRIs are recommended medications to treat panic attacks (Prozac, Zoloft)
- SNRIs (Effexor XR)
Social Anxiety Disorder (social phobia) Severe, persistent, and unreasonable fears of social or performance situations in which embarrassment may occur ● Performance only: talking, performing, eating or writing in public ● Broad: General fear of functioning poorly in front of others DSM-5 Checklist 1. Marked, disproportionate, and persistent fear of anxiety about one or more social situations where they are exposed to possible scrutiny 2. Fear of being negatively evaluated by or offensive to others 3. Anxiety is almost always produced by exposure to the social situation 4. Avoidance of feared situations 5. Significant distress or impairment They believe that ● They are socially unskilled and inadequate ● They are always in danger of behaving incompetently in social situations ● Inept behaviors in social situations will inevitably lead to terrible consequences Can greatly interfere with one's life (often kept a secret) ● 7% of people in the U experience a social anxiety disorder in any given year ● Women outnumber men 3: ● Phobias often begin in childhood and may persist for many years Cognitive Traps ● "Everyone else looks so much more relaxed" "What if I say something dumb" ● These thoughts start to rapidly spiral out of control to the point that anything anyone else has said is missed. People may say as little as possible and hope that no one has noticed their anxiety ● Negative beliefs: Strongly held beliefs about inadequacy in social and/or performance-related situations ● Mental filter: A tendency to discount positive social encounters and magnify the social abilities of others
Phobias-Etiology and Treatment
Etiology Behavioral models is the predominate reason Direct learning: Specific phobias can sometimes begin following a negative experience in the feared situation Observational learning: Some people may learn to fear certain situations by watching others show signs of fear Informational learning: Sometimes, people develop specific phobias after hearing reading about a situation that may be dangerous Classical conditioning: Some theories suggest that specific phobia may also develop due to an association of a specific object or situation with emotions such as fear and panic
A behavioral-evolutionary explanation ● Called "preparedness" because human beings are theoretically more prepared to acquire some phobias than others ● The model explains why some phobias (snakes and spiders) are more common than others ● Preparedness= inherited tendency to fear situations that have always been dangerous to the human race Treatment Systematic desensitization ● Teach relaxation skills ● Create fear hierarchy (stimulus hierarchy) ● Pair relaxation with the feared objects or situations ● Since relaxation is incompatible with fear, the relaxation response is thought to substitute for the fear response ● 1-5 sessions Other behavioral treatments: Flooding ● Nongradual exposure Modeling ● The therapist confronts the feared object while the fearful person observes The key to success is actual contact with the feared object or situation Reluctance ● People think their phobia is untreatable ● Most treatments involve direct contact with the phobic target ● Some individuals may have been unsuccessful in conducting self-administered exposure and concluded that they are unresponsive to this mode of treatment Medications for Anxiety Disorder Medications ● SSRIs (Zoloft and Paxil) ● SNRIs (venlafaxine)
Abnormal Psych Study Guide for Exam 1
Course: Abnormal Psychology (PSYC 3303)
University: University of Colorado Boulder

- Discover more from: