- Information
- AI Chat
Hemodynamic monitoring: why/ how/when/ nurses role
Nursing (01)
Kerala University of Health Sciences
Recommended for you
Related Studylists
med surg IIIPreview text
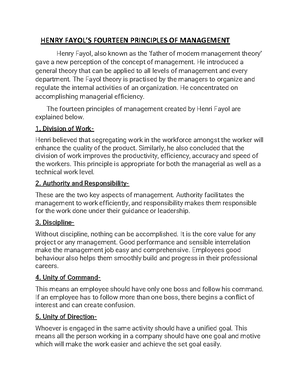
INTRODUCTION
Hemodynamic monitoring measures the blood pressure inside the veins, heart, and arteries. It also measures blood flow and how much oxygen is in the blood. It is a way to see how well the heart is working fundamentals of hemodynamic monitoring have changed very little over the past years. The main goal of hemodynamic monitoring in the critically ill patient remains the correct assessment of the cardiovascular system and its response to tissue oxygen demands monitoring is used to assess cardiovascular function in the critically ill patients.
DEFINITIONS
1 monitoring of the movement of blood and the pressure being exerted in the veins , arteries and chambers of the heart
- Hemodynamic monitoring is the expert collection and analysis of qualitative and quantitative data of cardio pulmonary fuction.
GOALS
To maintain adequate tissue perfusion To assure the adequacy of perfusion.
Early detection of an inadequacy of perfusion. To titrate therapy to specific hemodynamic endpoints in unstable patients. To differentiate among various organ system dysfunction's.
PURPOSES
-This test can find problems with how the heart is working. Treating problems early may prevent complications. This is very important for some people who need to have surgery or who are very sick.
-Early detection identification and treatment of lifethreatening conditions such as heart failure and cardiac tamponade.
-Evaluate patients immediate response to treatment
-Classical hemodynamic monitoring is based onn the invasive measurement of system ,pulmonary arterial and venous pressure of the cardiac out put.
INDICATIONS OF HEMODYNAMIC MONITORING
-Decreases cardiac output
-All types of shock
-Deficit or loss of cardiac function
-Need to assess left ventricular function
-To estimate patient prognosis
-Monitor cardiac performance
-Evaluate cardiac response to drugs
-Right ventricular infarction
-Mitral regurgitation
-Pulmonary embolism
-Potential or actual alteration in CO
-Potential or actual alteration in fluid volume
-Cvp monitoring
-Arterial pressure monitoring
-Pulmonary arterial pressure monitoring
The circulatory system consists of two parts: the pulmonary circulation, which is a low pressure system with low resistance to blood flow, and the systemic circulation, which is a high pressure system with high resistance to blood flow.
PRELOAD
Preload refers to the amount of myocardial fiber stretch at the end of diastole, it also refers to the amount of volume in the ventricle at the end of this phase. It is clinically acceptable to measure the pressure required to fill the ventricles as an indirect assessment of ventricular preload. Left atrial filling pressure or pulmonary artery wedge pressure is used to assess left ventricular preload. Right atrial pressure is used to assess right ventricular preload. Volumetric parameters provide a closer measurement to ventricular preload for the right ventricle.
AFTERLOAD
Afterload refers to the tension developed by the myocardium during ventricular systolic ejection. More commonly, afterload is described as the resistance, impedance, or pressure that the ventricles must overcome to eject their blood volumes. Afterload is dependent on a number of factors, including volume and mass of blood ejected, the size and wall thickness of the ventricles, and the impedance of the vasculature. In the clinical setting, the most sensitive measure of afterload is systemic vascular resistance (SVR) for the left ventricle and pulmonary vascular pressure (PVR) for the right ventricle.
Afterload has an inverse relationship to ventricular function. As resistance to ejection increases, the force of contraction decreases, resulting in a decreased stroke volume. As resistance to ejection increases, an increase in myocardial oxygen consumption occurs.
CONTRACTILLITY
Most forms of acute and chronic heart failure are characterized by an impairment of contractility, and many treatment options - like catecholamines and phosphodiesterase inhibitors - in the perioperative arena are targeted to improve contractility of the heart.
This is in contrast to the treatment of chronic heart failure, where afterload and preload reduction dominate, while positive inotropic measures are unwanted, with the exception of digitalis. Direct measurement of contractility by pressure volume curves is difficult in the clinical setting; indirect measures include echocardiographic determination of ejection fraction, measurement of cardiac output, stroke volume and right as well as left ventricular stroke work index in relation to systemic and pulmonary vascular resistance.
MONITORING TECHNIQUES
Hemodynamic monitoring using invasive techniques is the mainstay of today's practice of critical care and allows precise frequent determinations of cardiorespiratory variables. However, noninvasive measures should not be forgotten!
NON –INVASIVEBLOOD PRESSURE MONITORING METHODS
1 MONITORING
5 PRESSURE MONITORING
Peripheral arterial lines (A. radialis) offer several advantages in comparison of monitoring blood pressure with a cuff. The line provides continuous measurement of blood pressure and can be used for sampling of blood gases. A strong variation in the amplitude may indicate volume deficiency.
In the setting of marked vasoconstriction or hypotension, the arterial line gives more accurate pressure values than a blood pressure cuff; however, in case of strong centralization of circulation, blood pressure measurements done with peripheral arterial lines may considerably differ from the core hemodynamics.
Indications include
Rapidly changing clinical circumstances in critically ill patients (e. hemorrhage, sepsis). Monitoring and guiding the use of vasoactive drugs with rapid cardiovascular effects. Monitoring and guiding acute interventions (e. major surgery, resuscitation). Blood sampling.
COMPLICATIONS OF ARTERIAL CATHETERIZATION
-HEMORRHGE
-HEMATOMA
-THROMBOSIS
-PROXIMAL OR DISTAL EMBOLISATION
-PSEUDOANEURISM
-INFECTION
6 ARTERY CATHETER
The pulmonary artery catheter offers several advantages over central venous pressure monitoring. When the balloon tip of a Swan Ganz catheter is properly wedged in a branch of the pulmonary artery, the pressure sensed by the catheter tip represents that in the left atrium, taking aside a specific problem of pulmonary capillary wedge pressure monitoring in the septic patient.
COMPLICATIONS OF PULMONARY ARTERY CATHETERIZATION
General central line complicationsPneumothorax -Arterial injury -Infection -Embolization
Inability to place PAC into PA
Arrhythmias (heart block) Pulmonary artery rupture
7 ECHOCARDIOGRAPHY
Echocardiography is making major inroads into the critical care units. In general, physical examination of critically ill cardiac patients is limited in its accuracy in predicting measured physiologic data. Available studies suggest that protocol-driven pulmonary artery catheter management will modify central venous pressure driven management some 40% of the time, with strong suggestions of improvement in outcome. Recent data suggest that in patients with pulmonary artery catheter-driven care, the use of TEE modifies management another 40% of the time. Diagnosis of many disease processes and pathophysiologic derangements are beyond the capabilities of routine invasive monitoring techniques and can only be made by bedside echocardiography.
Since its introduction in the early eighties, echocardiography has undergone a huge technological and clinical evolution. The indications of echocardiography as a diagnostic and monitoring tool in the peri-operative and critical care setting have increased exponentially because of its potential to accurately assess cardiovascular dynamics. TEE is able to assess global and regional left ventricular function and can reliable evaluate the different determinants of ventricular function such as preload, contractility and afterload. The short axis view of the left ventricle is a basic and readily available part of this imaging technique. Moreover, its adequate visualization of the great vessels leads to an appreciation of cardiovascular interaction and helps to differentiate between cardiac and vascular causes of hemodynamic disturbances.
The hemodynamic monitoring includes
Clinical observation Use of electrical photometric Pressure transducing equipment Non invasive devices Applications of intravascular catheters
PARAMETERS INCLUDED IN HEMODYNAMIC MONITORI
NG
EQUIPMENT AND MATERIALS
-Appropriate apparel for asceptic technique and universal precautions (gowns , gloves ,caps ,masks etc )
-Cardiao respiratory monitor , printer , ECG
-Pulse oximeter
-Arterial catheter
-Wrist immobilizer
-1% Lidocaine
-0%NACL and Heparanised 0% NACL
-25 Gauge needle and syringe
-One –inch tape
-Sterile dressings
-Fluid –filled monitoring system
-Pulmonary artery catheter kit
-Betadine
-Introduce pump infusionset-up
-Thermodilusion cardiac output cable with module
-Ice bucket filled with ice
-Blood gas analysis syringe
-Manual resuscitator , mask intubation box
COMPONENTS OF THE MONITORING EQUIPMENTS
An invasive hemodynamic monitoring system has five basic components
- Monitor
- Flush system
- Transducer
- High pressure tubings
- Catheter
PROCEDURE
Assistance with insertion of invasive lines for hemodynamic monitoring purpose
Assemble all equipments and materials The choice of flush solution for the maintanence of patency of invasive lines is based on the patient’s blood count If thrombocytopenia is not a problem ,solution of heparin in 0% NaCl should be used Assemble fluid filled monitoring system and run the flush solution through all lengths of tubings ,stopcocks and side ports so as to remove all air from the system. Place “dead end” caps on all of the ports to maintain asepsis. Label the flush bags and lines with appropriate label ,date time and of set up Pump up the pressure infusor bags to 300 mm hg. Attach monitor cable and level of the pressure wave forms on the cardio respiratory monitor Level the transducer to the level of patients phlebostatic axis and zero the lines For bolus thermodilusion cardiac output , place 5% dextrose solution injectates in the ice ,fill the reference text tube with water and place the reference tube in the ice also For the use of the vigilance system ,, plug the monitor in to a grounded ACpower outlet and turn the monitor ON. Connect the interfacing cables including the topical module into front of the monitor Allow 20 minutes for optical module warm-up before beginning continous monitoring
INSERTION OF PULMONARY ARTERY CATHETER
1 the special procedure kit ,the physician will secure the flush lines for attatchment to the pulmonary artery distal part and the central venous proximal part 2 the physician to attatch a stop cock followed by a flush line to the auxillary part of the catheter 3 the line 4 the physician to remove the flush line from the auxillary part while maintaining 5 there and turning the stopcock off to the catheter 6 the catheter until solution is observed at the right atrial proximal part on the catheter
7 the physician to attatch the second flush line to the pulmonary artery distal part using stop cock. 8 that the physician inflates the balloon to check for patency and symmetry. 9 sleeves for post insertion manipulation of the catheter to the hub of the catheter 10 that the pressure monitoring lines are labeled correctly and that transducers are level with for patients phlebostatic axis and zeroed 11 the pulmonary arterial wave form on the cardiorespiratory monitor utilizing the 0- 30 mm hg pressure scale 12 the printer 13 ensure the accuracy of monitored preesure , a quality check of the system must be performed prior to data collection. 14 a hard copy of all pressure waveforms being monitored atleast once per 12 hours shift. 15 hard copies for arterial, central venou s , pulmonary artery , and pulmonary artery wedge pressure .these are obtained in a supine flat position. 16 an average for the cardiac output using the manual thermodilusion method 17 arterial and mixed venous blood for blood gas analysis
POST PROCEDURE Ensure that five additional injectates are inserted into the ice bucket and replace ice as needed Ensure that the proper pressure waveforms are displayed on the monitera after manipulations to the flush lines or catheters Return the patient to a comfortable position after the data collection and relevel all transducers Report the total volume of fluid used for the cardiac output determination Change the flush bags daily and change flush lines and transducers every 72 hours Non disposable items of hemdynamic monitoring should be wiped down with alcohol after use and before storage Inspection and testing of the system is performed once per shift at a minimum Record all data generated through hemodynamic monitoring on the patient daily record Report all information pertinent to the patient’s hemodynamic status as well as that information pertinent to data collection (patient position , catheter locked , tolerance ) Record line insertion later ,flush solution type Chart removal of the arterial catheter
Pulmonary infarction Knotting , looping of pulmonary artery catheter in the vessels or chamber of the heart
PRECAUTIONS
-Use asceptic techniques
-Monitors and equipments must be in good working conditions
-Pulmonary artey catheters should be monitored continuously
-Appropriate pressure and alarms should be maintained throughout monitoring
-If hemorrhage occur apply direct pressure
-Fluid filled monitoring systems must be assesses for optimal function before data collection and analysis
-Guidelines for the Prevention of Intravascular Catheter-Related Infections
GUIDELINES FOR THE PREVENTION OF INTRAVASCULAR
CATHETERR –RELATED INFECTIONS
Hand Hygiene : Thorough handwashing prior to insertion or handling of central venous catheters will reduce risk of nosocomial infections.
Maximal Barrier Protection : The insertion of a central venous catheter should be done under sterile (surgical asepsis) conditions. The clinician inserting the catheter should wear mask, cap, sterile gloves, and sterile gown. The patient should be draped in a sterile field around the insertion site. Assistants (e., nurses) should wear masks, protective gowns, and gloves while in the area–if the nurse will be working with the sterile equipment or supplies, the nurse should wear sterile gown, mask, cap, and sterile gloves too.
Chlorhexidine Skin Antisepsis : Chlorhexidine has been shown to reduce more skin normal flora than povidone-iodine or alcohol as a skin disinfectant prep prior to insertion of a central venous line.
Optimal Catheter-Site Selection : Rates of catheter-related bloodstream infections are lowest among catheters inserted into subclavian vein compared to internal jugular vein. Femoral vein insertions should be avoided if possible due to the high rates of bloodstream infections associated with the inguinal area.
Daily Medical Review of Necessity of Catheter : The medical physician should review daily the need for a central venous catheter with the goal of early removal as soon as the patient no longer needs the catheter. The longer a catheter is retained, the higher the probability of bloodstream infection. The nurse can bring this to the physician's attention during rounds as to whether any critical interventions like TPN or hemodynamic monitoring is occurring that needs a central venous catheter.
Replacement of Catheter : Recent evidence suggests that the rate of infections are not significantly different when catheters are replaced every 72 hours or les
BUNDLE OF PRACTICES RELATED TO NURSING CARE
All-Inclusive Catheter Cart or Kits : Having a cart or kit that has all necessary equipment for procedures reduces the risk of contamination of equipment when additional items are added to a sterile field.
Hand Hygiene : For all nursing procedures involving a central venous catheter (changing tubing, adding second infusion line, changing TPN solutions, IV administration of medication) the nursing care should begin with thorough hand washing with soap and running water to reduce the risk of nosocomial infections from other sources.
Site Care : Maintain a well adhesive transparent dressing over central venous catheters. Cath cares should involve scrubs of site with chlorhexidine during dressing changes. Transparent dressings only need to be changed every 7 days. Gauze dressings should be changed every 48 hours. Anytime a dressing is damp, soiled, or coming loose, then it should be changed with a full skin prep prior to application of a new dressing.
Line Access : The less frequently a central line is accessed from one of its ports (hubs), the higher the risk of a bloodstream infection. Therefore, do not access a central venous catheter except for essential procedures requiring the central line.
Scrub the Hub : When a hub on a central venous catheter infusion line is accessed, evidence does not support chlorhexidine over 70% isopropyl alcohol. However, the duration of scrubbing the access hub influences the risk significantly reduces bloodstream infections.
Replacement of IV Administration Sets (Tubing): Replacement of central line tubing every 72 hours is not associated with lower infection rates compared to 96 hours. Replacement of
Hemodynamic monitoring: why/ how/when/ nurses role
Course: Nursing (01)
University: Kerala University of Health Sciences

- Discover more from: