- Information
- AI Chat
Summary of Bates’ Guide to Physical Examination and History Taking (12th Edition)
Bachelors in Science in Nursing (NCA)
Ateneo de Zamboanga University
Recommended for you
Preview text
Bates’ Guide to Physical Examination and History Taking (12th Edition)
Bates’ Guide to
Physical
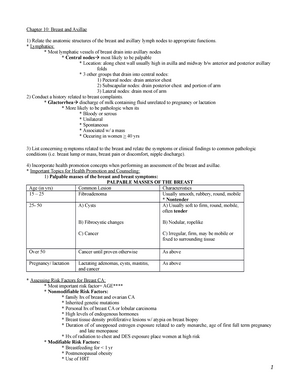
Examination and
History Taking
( 12
th
Edition)
Bates’ Guide to Physical Examination and History Taking (12th Edition)
Unit 1:
Foundations of
Health
Assessment
Chapter 1: Foundations for Clinical Proficiency
Chapter 2: Evaluating Clinical Evidence
Chapter 3: Interviewing and the Health History
Bates’ Guide to Physical Examination and History Taking (12th Edition)
The History and Physical Examination: Type of Assessment COMPREHENSIVE ASSESSMENT FOCUSED/ PROBLEM – ORIENTED ASSESSMENT ▪ Is appropriate for new patients in the office or hospital ▪ Provides fundamental and personalized knowledge about the patient ▪ Strengthens the clinician–patient relationship ▪ Helps identify or rule out physical causes related to patient concerns ▪ Provides a baseline for future assessments ▪ Creates a platform for health promotion through education and counseling ▪ Develops proficiency in the essential skills of physical examination ▪ includes all the elements of the health history and the complete physical examination
▪ Is appropriate for established patients, especially during routine or urgent care visits ▪ Addresses focused concerns or symptoms ▪ Assesses symptoms restricted to a specific body system ▪ Applies examination methods relevant to assessing the concern or problem as thoroughly and carefully as possible ▪ for patients who are returning for routine care ▪ patients who need specific urgent care (ex. Knee pain or Sore Throat)
####### COMPREHENSIVE EXAMINATION FOCUSED/ PROBLEM – ORIENTED EXAMINATION
▪ Does more than assess body systems ▪ It is a source of fundamental and personalized knowledge about the patient that strengthens the clinician–patient relationship ▪ Most people seeking care have specific worries or symptoms. ▪ The comprehensive examination provides a more complete basis for assessing these concerns and answering patient questions
▪ select the methods relevant to thorough assessment of the targeted problem ▪ The scope of the Focused Examination is determined by: 1. The patient’s symptoms 2. Age 3. health history help 4. Our knowledge of disease patterns
Subjective VS Objective Data/ Information
Knowing these differences helps you group together the different types of patient information. These distinctions are equally important for organizing written and oral presentations about patients into a logical and understandable format
####### SUBJECTIVE DATA/ INFORMATION OBJECTIVE DATA/ INFORMATION
▪ Symptoms and history o what patients tell you o from Chief complaint through Review of Systems
Signs – What you observe/ detect during the P., Lab results, and test data (all examination findings and signs)
####### EXAMPLE
Mrs. G. is a 5 4 - year-old hairdresser who reports
pressure over her left chest “like an elephant sitting
there,” which goes into her left neck and arm.
Mrs. G. is an: Old, overweight white female, who is pleasant and cooperative. Height 5′ 4 ′′ Weight 150 lbs BMI 26 BP 160/ HR 96 Regular, Respiratory Rate @ 24 Temperature 97 °F
Bates’ Guide to Physical Examination and History Taking (12th Edition)
The Comprehensive Adult Health History
Components of the Comprehensive Health History
o Identifying data and source of the history; reliability o Chief complaint(s) o Present illness o Past history o Family history o Personal and social history o Review of systems ▪ you will closely follow the patient’s cues: - to elicit the patient’s narrative of illness - provide empathy - and strengthen rapport
OVERVIEW: COMPONENTS OF THE ADULT HEALTH HISTORY
IDENTIFYING DATA AND SOURCE OF
THE HISTORY
▪ Identifying data—such as age, gender, occupation, marital status ▪ Source of the history —usually the patient, but can be a family member or friend, letter of referral, or the clinical record ▪ If appropriate, establish the source of referral, because a written report may be needed
RELIABILITY Varies according to the patient’s memory, trust, and mood
CHIEF COMPLAINT(S) The one or more symptoms or concerns causing the patient
to seek care
PRESENT ILLNESS ▪ Amplifies the Chief Complaint; describes how each
symptom developed ▪ Includes patient’s thoughts and feelings about the illness ▪ Pulls in relevant portions of the Review of Systems, called “pertinent positives and negatives” ▪ May include medications, allergies, and tobacco use and alcohol, which are frequently pertinent to the present illness
PAST HISTORY ▪ Lists childhood illnesses
▪ Lists adult illnesses with dates for events in at least four categories: o Medical o Surgical o Obstetric/Gynecologic o Psychiatric ▪ Includes health maintenance practices such as immunizations, screening tests, lifestyle issues, and home safety
FAMILY HISTORY ▪ Outlines or diagrams age and health, or age and
cause of death, of siblings, parents, and grandparents ▪ Documents presence or absence of specific illnesses in family, such as hypertension, diabetes, or type of cancer
PERSONAL AND SOCIAL HISTORY ▪ Educational level
▪ Family of origin ▪ Current household ▪ Personal interests ▪ Lifestyle
Bates’ Guide to Physical Examination and History Taking (12th Edition)
Route of administration Frequency of use
▪ Ask patients to bring in all their medications so that you can see exactly what they take
Vitamins Mineral or Herbal Supplements Oral Contraceptives Medicines Borrowed from Others
NOTE ALLERGIES TOBACCO USE ALCOHOL and DRUG USE ▪ including specific reactions to each medication o rash or nausea ▪ allergies to o foods o insects o environmental factors
▪ including the type of cigarette ▪ Cigarettes are often reported in pack years ▪ (a person who has smoked 1½ packs a day for 12 years has an 18-pack/ year history). ▪ If someone has quit, note for how long
e should always be investigated and is often pertinent to the Presenting Illness
PAST HISTORY
Childhood Illnesses ✓ MEASLES ✓ MUMPS ✓ RUBELLA ✓ WHOOPING COUGH ✓ CHICKENPOX ✓ RHEUMATIC FEVER ✓ SCARLET FEVER ✓ POLIO
Include also any chronic
childhood illnesses
Adult Illnesses MEDICAL SURGICAL OBSTETRICS/ GYNECOLOGIC PSYCHIATRIC ( 1 ) Illnesses such as diabetes, hypertension, hepatitis, asthma, and human immunodeficiency virus (HIV) (2) Hospitalizations ( 3 ) Number and gender of sexual partners (4) risk-taking sexual practices
( 1 ) Dates (2) Indications ( 3 ) Types of operations
( 1 ) Obstetric history (2) Menstrual history ( 3 ) Contraception Methods (4) sexual function
( 1 ) Illness and time frame, diagnoses (2) hospitalizations ( 3 ) Treatment
Provide information relative to Adult Illnesses in each of the four areas.
Health Maintenance IMMUNIZATIONS (Received vaccines) SCREENING TESTS
✓ Tetanus
✓ Pertussis (whooping cough)
✓ Diphtheria
✓ Polio
✓ Measles (Rubeola)
✓ Rubella (German measles)
✓ Mumps
✓ Influenza
✓ Varicella (chickenpox)
✓ Hepatitis B virus (HBV)
✓ Human Papilloma Virus (HPV)
✓ Meningococcal Disease
✓ Haemophilus Influenzae type B
✓ Tuberculin Tests ✓ Pap Smears (pap test or Papanicolaou Test) ✓ Mammograms ✓ Stool Tests for Occult Blood ✓ Colonoscopy ✓ Cholesterol Tests
▪ Include and gather the Results and When they were last performed.
Bates’ Guide to Physical Examination and History Taking (12th Edition)
✓ Pneumococci
✓ Herpes Zoster
####### FAMILY HISTORY
####### PERSONAL AND SOCIAL HISTORY
- the patient’s personality and interests
- sources of support and coping style
- strengths
- concerns
- occupation
- home situation and significant others
- sources of stress, both recent and long-term
- important life experiences
- job history
- financial situation and retirement
- leisure activities
- religious affiliation and spiritual beliefs
- Baseline level of function is particularly important in older or disabled patients.
- Lifestyle habits
- activities of daily living (ADLs) o That Promote health or create risk ▪ Exercise and its frequency ▪ Diet and daily food intake ▪ Dietary Supplements or Restrictions ▪ Safety Measures ▪ Sexual Orientaion ▪ Exposure to any practices of alternative health practices ▪ Personalizes your relationship with the patient and build rapport
REVIEW OF SYSTEMS (TIPS on How to Approach Questioning) 1. Think about asking a series of questions going from “head to toe.” 2. Note that as you elicit the Present Illness, you may also draw on Review of Systems questions related to system(s) relevant to the Chief Complaint to establish “pertinent positives and negatives” that help clarify the diagnosis. - Example: After a full description of chest pain, you may ask: o “Do you have any history of high blood pressure... palpitations... shortness of breath... swelling in your ankles or feet?” ▪ or even move to questions from the Respiratory or Gastrointestinal Review of Systems
Family History
Parents Grandparents Siblings Children Grandchildren
####### ALIVE
####### DECEASED
Present or Absent Conditions and Records in the Family
Hereditary Diseases
History Of Cancer
Age & Cause of Death
Age and Health Condition
Hypertension Coronary Artery Disease Elevated Cholesterol Levels Stroke Diabetes Thyroid Or Renal Disease Arthritis Tuberculosis Asthma Or Lung Disease Headache Seizure Disorder Mental Illness Suicide Substance Abuse Allergies
Breast Cancer Ovarian Cancer Colon Cancer Prostate Cancer
Bates’ Guide to Physical Examination and History Taking (12th Edition)
▪ Rheumatic Fever ▪ Heart Murmurs ▪ Chest Pain Or Discomfort ▪ Palpitations Shortness Of Breath ▪ Need Pillows At Night To Ease Breathing (Orthopnea)
(Paroxysmal Nocturnal Dyspnea) ▪ Swelling In The Hands, Ankles, Or Feet (Edema) ▪ Results Of Past Electrocardiograms Or Other Cardiovascular Tests
GASTROINTESTINAL
▪ Trouble Swallowing ▪ Heartburn ▪ Appetite ▪ Nausea ▪ Bowel Movements and Constipation ▪ Stool Color and Size ▪ Change in Bowel Habits ▪ Pain With Defecation Rectal Bleeding ▪ Hemorrhoids
▪ Diarrhea ▪ Abdominal Pain ▪ Food Intolerance ▪ Excessive Belching or Passing of Gas. ▪ Jaundice ▪ Liver or Gallbladder Trouble ▪ Hepatitis ▪ Black or Tarry Stools
PERIPHERAL VASCULAR
▪ Intermittent Leg Pain With Exertion (Claudication) ▪ Leg Cramps ▪ Varicose Veins ▪ Past Clots In The Veins ▪ Swelling In Calves, Legs, or Feet ▪ Color Change In Fingertips Or Toes During Cold Weather ▪ Swelling With Redness Or Tenderness.
URINARY
▪ Frequency of urination ▪ Urgency of urination ▪ Polyuria ▪ Nocturia ▪ burning or pain during urination ▪ blood in the urine (hematuria) ▪ urinary infections ▪ kidney or flank pain ▪ kidney stones ▪ ureteral colic
▪ suprapubic pain ▪ incontinence
In males: ▪ reduced caliber or force of the urinary stream ▪ hesitancy ▪ dribbling
GENITAL
Male
▪ Hernias ▪ Discharge From or Sores On The Penis ▪ Testicular Pain or Masses ▪ Scrotal Pain or Swelling ▪ History of STI and Tx
▪ Sexual habits, interest, function, and satisfaction ▪ birth control methods ▪ condom use, and problems ▪ Concerns about HIV infection
Female
Age at menarche
▪ Menstruation: - Regularity - Frequency - Duration ▪ Amount of bleeding ▪ Bleeding between periods or after intercourse ▪ Last menstrual period ▪ Dysmenorrhea
If the patient was born before 197 1, exposure to DIETHYLSTILBESTROL (DES) from maternal use during pregnancy (linked to cervical carcinoma)
▪ Vaginal Discharge ▪ Itching ▪ Sores ▪ Lumps ▪ Sexually transmitted infections and treatments
▪ Number of pregnancies
Bates’ Guide to Physical Examination and History Taking (12th Edition)
▪ Premenstrual tension
Age at menopause ▪ Menopausal symptoms ▪ Postmenopausal bleeding
▪ Number and type of deliveries ▪ Number of abortions (spontaneous and induced) ▪ Complications of pregnancy ▪ Birth-control methods ▪ Sexual preference, interest, function, satisfaction ▪ Dyspareunia ▪ Concerns about hiv infection
MUSKOLOSKELETAL
▪ Muscle or joint pain ▪ stiffness ▪ Arthritis ▪ Gout ▪ Backache
If present, describe location of affected part
Joints or Muscles that have: ▪ Swelling and Redness ▪ Pain ▪ Tenderness ▪ Stiffness ▪ Weakness ▪ limitation of motion or activity
Include timing of symptoms (e., morning or evening) duration any history of trauma
▪ Neck or low back pain
Joint pain with systemic symptoms such as: ▪ Fever ▪ Chills ▪ Rash ▪ Anorexia ▪ Weight loss ▪ Weakness
PSYCHIATRIC
▪ Nervousness ▪ Tension ▪ Mood ▪ Depression
▪ memory change ▪ suicidal ideation ▪ suicide plans or attempts
▪ Past counseling ▪ Psychotherapy ▪ psychiatric admissions.
NEUROLOGIC
Changes in: - Mood - Attention - speech - orientation - memory - insight - judgment
▪ headache ▪ dizziness ▪ vertigo ▪ fainting ▪ blackouts ▪ weakness ▪ paralysis
▪ numbness or loss of sensation, tingling or “pins and needles ▪ tremors or other involuntary movements ▪ seizures
HEMATOLOGIC
▪ Anemia ▪ easy bruising or bleeding
▪ past transfusions ▪ transfusion reactions
ENDOCRINE
▪ “Thyroid trouble” ▪ heat or cold intolerance ▪ excessive sweating
▪ excessive thirst or hunger ▪ polyuria ▪ change in glove or shoe size
Bates’ Guide to Physical Examination and History Taking (12th Edition)
- A reflex hammer
- Tuning forks, both 12 8 Hz and 5 12 Hz
- Cotton swabs, safety pins, or other disposable objects for testing sensation and two-point discrimination
- Cotton for testing the sense of light touch
- Two test tubes (optional) for testing temperature sensation
- Gloves and lubricant for oral, vaginal, and rectal examinations
- Vaginal specula and equipment for cytologic and bacteriologic studies
- Paper and pen or pencil, or desktop or laptop computer
Make the patient comfortable and protect their privacy
- be modest and sensitive because patients’ feels vulnerable during assessment
- close nearby doors, windows, draw the curtains and must follow strict handwashing before and after.
- Be aware of any discomfort and feelings of the patient
- Are you okay? Or Is this painful?” – common phrases to show care
- Give Courteous Clear Instructions
- Keep the patient informed
- Ask beforehand if she wants to know the findings (is she curious about what are you doing?) Observe standard and universal precautions
Follow the guidelines of the CDC (Center for Disease Control and
Prevention (CDC)
Choose the sequence, scope, and positioning of examination
Bates’ Guide to Physical Examination and History Taking (12th Edition)
Summary of Bates’ Guide to Physical Examination and History Taking (12th Edition)
Course: Bachelors in Science in Nursing (NCA)
University: Ateneo de Zamboanga University
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades

This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades
Why is this page out of focus?
This is a preview
Access to all documents
Get Unlimited Downloads
Improve your grades