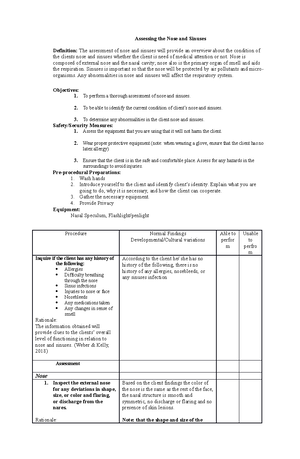
- Information
- AI Chat
Was this document helpful?
Health Care Plan
Course: Nursing
999+ Documents
Students shared 5712 documents in this course
University: Bukidnon State University
Was this document helpful?

Health Care Plan
Prevention and/or infection control for open wounds
I. Outcomes/Objectives:
After 2 hours health teaching and nursing intervention, everyone will be able to:
1. Demonstrate and discuss open wound for them to have a knowledge of what and why we should do an action to
prevent infection in open wounds. (Cognitive domain)
2. Identify what are the supplies to be use, Perform and practice the procedures with the participants step-by-step
as it follows. (Psychomotor domain)
3. Assist the participates in the circumcision care and let them express themselves. (Affective domain)
II. Formulate a plan Strategies Evaluation Learning Situation:
After 2 hours of health teaching and nursing intervention, the participants will be able to perform the procedure and
assess its patient in the given drill situation.
III. Strategies:
1. Discussion of concept for infection prevention and control:
Wound care treatments and services provided in the long-term care setting can entail complex procedures
utilizing a wide array of products and/or equipment. The following wound care infection prevention and control
recommendations are designed to assist long-term care facilities with general principles and are not all-inclusive.
Hand hygiene:
Perform hand hygiene before starting wound care for each resident (including before retrieving wound care
supplies and before donning gloves), and after doffing gloves.
Alcohol hand rub should be readily accessible throughout the wound care process. Ways to ensure this include
keeping an alcohol hand rub close to the bed (point of care) in the room when performing wound care in
addition to placing alcohol hand rub dispensers in the hallway outside resident rooms.
Personnel should not touch items in the resident care environment while performing wound care as this will
contaminate gloves and/or the environment.
Personal Protective Equipment:
Keep gloves available in all sizes for staff and providers.
Wear gloves during all stages of wound care including when applying new dressings. Don them after
preforming hand hygiene. During an individual resident’s treatment, doff gloves every time when going from
dirty to clean surfaces or supplies and before caring for another resident.
Wear a mask with eye protection if there is any chance of splattering (e.g., wounds with drainage, especially
during debridement and irrigation).
Wear a new disposable gown to cover arms and clothing that may come in contact with the resident or the
resident’s bed for each dressing change. *Because it typically cannot be predicted ahead of time if health care
workers or their clothing may come in contact with the wound or drainage, health care workers should consider
wearing gowns for all wound care. Some exceptions could be made for patients with small, non-draining
wounds, which do not require any hands-on contact with the patient (including positioning the patient) or
bedding.
2. Skills Demonstration on proper wound care:
Wound Care Aid
1. Control bleeding:
- Gently rinse the wound with clean, lukewarm water to cleanse and remove any fragments of dirt, e.g.
gravel, as this will reduce the risk of infection.
2. Wash your hands well:
- Prior to cleaning or dressing the wound, ensure your hands are washed to prevent contamination and
infection of the wound.
3. Rinse the wound:
- Gently rinse the wound with clean, lukewarm water to cleanse and remove any fragments of dirt, e.g.
gravel, as this will reduce the risk of infection.
4. Dry the wound
- Gently pat dry the surrounding skin with a clean pad or towel.
5. Replace any skin flaps if possible
- If there is a skin flap and it is still attached, gently reposition the skin flap back over the wound as
much as possible using a moist cotton bud or pad.
6. Cover the wound
- Use a non-stick or gentle dressing and lightly bandage in place; try to avoid using tape on fragile skin
to prevent further trauma on dressing removal.