- Information
- AI Chat
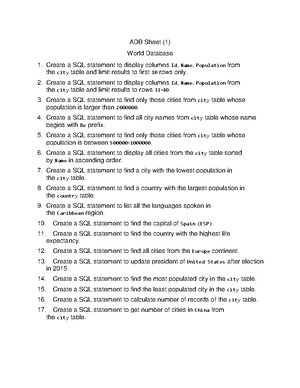
Topographic Anatomy
Anatomy 1
Assiut University
Preview text
O. V. Korencov, G. F. Tkach
TOPOGRAPHIC ANATOMY OF THE HEAD
Study guide
Ministry of Education and Science of Ukraine
Ministry of Health of Ukraine
Sumy State University
O. V. Korencov, G. F. Tkach
TOPOGRAPHIC ANATOMY OF THE HEAD
Study guide
Recommended by Academic Council of Sumy State University
Sumy
Sumy State University
2016
TOPOGRAPHIC ANATOMY OF THE HEAD
The head is subdivided into two following departments: the brain and facialohes. They are shared by line from the glabella to the supraorbital edge along the zygomatic arch to the outer ear canal. The brain part consists of fornix and base of the skull. The fornix is divided into fronto- parieto-occipital region, paired temporal and mastoid area. The facial region consists of frontal and lateral area. Regions of the frontal area include nasal, orbital, oral, mental regions. Regions of the lateral area include buccal and parotideomasseteric regions.
FRONTO-PARIETO-OCCIPITAL REGION
Borders:
- in front– supraorbital edge of the frontal bone;
- behind – external occipital protuberance and the upper nuchal line;
- sideways – superior temporal line. Layers: The skin is thick, covered by hair. It has sweat and sebaceous glands. Sebaceous cysts or atheroma are formed by blockage of the sebaceous gland ducts or by swelling of the hair follicle which then disrupts the emptying of the sebaceous gland through the pore. Folliculitis is a superficial infection of single hair follicles. A carbuncle is a deeper skin infection that involves a group of infected hair follicles in one skin location. Skin is firmly adherent to the subcutaneous tissue, m. epicranius and aponeurotic helmet because it has vertical connective tissue septa. Connective tissue septa divide the subcutaneous tissue into separate cells which are filled by fat. (The septa divide fat cells in the subcutaneous layer into columns). Therefore hematoma in this region has the form of limited swelling. In the subcutaneous tissue of the frontal region are:
- supratrochlearis;
- supraorbitalis;
- ophthalmica-branch of the internal carotid artery system. A. supratrochlearis comes out of the orbit through the incisura frontalis to the intersection of the supraorbital margin with vertical line drawn through the medial corner of the eye. A. supraorbitalis comes out of the orbit through the foramen supraorbitalis or incisura supraorbitalis between the middle and medial parts of margo supraorbitalis. Its terminal
branches anastomose with branches of the supratrochlear artery and the superficial temporal arteries. Outflow of venous blood is carried out by the v. supratrochlearis, v. supraorbitalis that flow into v. angularis. Vessels escort the nerves of the same name, branch n. frontalis from n. ophthalmicus. There are also rr. temporales from n. facialis, that innervat the venter frontalis of m. epicranius and m. orbicularis oculi, so their damage causes lagophthalmos "rabbit eye" − the eye is open and tearing. The lymphatic vessels of the frontal region are sent to nodi lymphatici parotidei superficialis et profundi. In the parietal area in the subcutaneous tissue are: - a/v. temporalis superficialis; - n. auriculotemporalis. A. temporalis superficialis is the terminal branch of the external carotid artery. It is located in front of the tragus of the auricle. It can be pressed to the bone to stop bleeding. V. temporalis superficialis is located near the same artery. It flows into v. retromandibularis and accepts v. emissaria parietalis. N. auriculotemporalis is a branch of n. mandibularis. It is accompanied the temporal artery and located in front of the vessels. Lymph flow is carried out in nodi lymphatici retroauricularis. In the subcutaneous tissue of the occipital region are: - a/v. auricularis posterior; - a/v. occipitalis; - n. occipitalis major/minor; - n. auricularis posterior. A. auricularis posterior is projected onto the skin on the posterior edge of the attachment of the auricle. A. occipitalis is projected in the middle of the distance between the mastoid process and occipital protuberance. Arteries are accompanied by the veins of the same name that flow into v. jugularis externa. The skin of the occipital region is innervated by major and minor occipital nerves. N. occipitalis major is a posterior branch of the second cervical nerve. It accompanies the occipital artery of n. occipitalis minor from the cervical plexus and passes 3 cm behind from the attachment of the ear. It is located at the rear edge of the m. sternocleidomastoideus, near mastoid process. N. auricularis posterior is a branch of n. facialis. It passes in the subcutaneous tissue behind the auricle and innervates the muscle of the same name, venter occipitalis and m. epicranius. Lymphatic vessels flow into nodi lymphatici occipitales.
PARTICULAR QUALITIES OF BLOOD FLOW
- v. emissaria mastoidea connects sinus sigmoideus with v. auricularis posterior. The links between the superficial and deep veins facilitates the outflow of blood from the brain at increased intracranial pressure or at obstruction to the main way. Besides, they can cause the penetration of infection at injury and diseases of the soft tissue of the cranial vault (furuncle) into the bone with the development of osteomyelitis, on the dura mater with the development of meningitis, brain abscess, sinus thrombosis. Such retrograde (in the reverse way) blood flow with the spreading of infection is possible due to the lack valve head in veins. Next layer is m. epicranius. Venter frontalis and venter occipitalis of m. epicranius connect tendon helmet. This layer of fibrous membranes is strongly linked with the skin. Thus, skin, subcutaneous tissue and tendon helmet are integrated and are a part of the flap at the scalped head injuries. There is subgaleal fiber under the tendon helmet. It doesen’t have any membranes. The scalped injuries in the cranial vault are possible due to a strong link of the skin with tendon helmet and with the periosteum. Hematomas and suppurative processes in the subgaleal tissue look like spilled swelling and occupy the entire surface of the cranial vault. The next layer is the periosteum. The periosteum is firmly soldered to the bones in the joints and loose on other sites. One should treat carefully to the periosteum at operations, because it consists of the vessels feeding lamina externa of the skull bones. The subperiosteal tissue is located deeper. The periosteum is easily scaled off, and hematomas are limited with line of bones and joints and are located within the separate bone due to the subperiosteal tissue. The subperiosteal hematomas disrupt the blood flow to the bones and they can lead also to necrosis of the outer part of the cranial vault. Therefore we remove them. All cellular spaces of fronto-parieto-occipital region are linked with each other through the anastomoses of external veins, sinuses of the dura mater and diploic veins through emissary veins. They can serve as pathways of inflammatory processes. Bone basis of the region form the frontal, occipital and parietal bones. They are connected to each other by means of ligamentous joints. The bones are plane, their inner surface is smooth and it has holes for vessels. Their inner surface is rough, has grooves and recesses from arteries, sinuses of the dura mater, granulation and gyri. Bones of the skull are composed of three layers.
- Lamina externa, the outer bone plate, consists of solid substance.
- The second layer – diploe, in intraosseous diploic channels of which
(Bréchet channels) vv. diploicae are located. 3. The third layer is the inner bone plate − lamina interna. It is more thin and brittle and that’s why is called the vitreous − lamina vitrea. It is broken oftener than the outer lamina. And it is broken with the formation of plenty of fragments. Its fragments often damage the vessels of the dura mater and the substance of the brain causing the epidural or subdural hematomas. Cranial bones regenerate slowly. So, it is possible to observe the bone defects on the X-ray photographies of the skull bones on the former site of fracture. In the frontal region between the outer and inner plates is the frontal sinus. The injury of frontal bone is subjected to a secondary infection of the nasal cavity.
TEMPORAL REGION Borders:
- from above and behind − superior temporal line;
- from below − zygomatic arch;
- in front − the frontal process of the zygomatic bone and the zygomatic process of the frontal bone. Layers: I. The skin is thin. It is covered with hair. The skin is innervated by n. auriculotemporalis, n. zygomaticotemporalis and n. occipitalis minor. II. Subcutaneous layer is small. It consist of:
- mm. auricularis anterior et superior;
- a./v./n. temporalis superficialis;
- n. zygomaticotemporalis;
- a./v. auricularis posterior;
- n. occipitalis minor. Mm. auricularis anterior et superior are innervated by rr. temporales of facial nerve. A. temporalis superficialis is accompanied by the v. temporalis superficialis and n. auriculotemporalis. n. zygomaticotemporalis, a branch of n. zygomaticus from n. maxillaris passes at the outer edge of the orbit. A. auricularis posterior, v. auricularis posterior and n. occipitalis minor are behind the auricle. The superficial fascia has the form of a thin plate. It is the extension of the tendon helmet. The superficial fascia forms a fascial sheath for the muscles of the ear, blood vessels and nerves. The own temporal fascia or the temporal aponeurosis splits into superficial and deep plate before the zygomatic arch. The surface plate of the own
There are:
- a. auricularis posterior;
- v. auricularis posterior;
- lymphatic vessels and nodes (nodi lymphatici mastoidei, which are linked with lymph from the auricle and parietal area);
- n. auricularis magnus;
- n. occipitalis minor;
- m. auricularis posterior, which are innervated by n. auricularis posterior, branch of n. facialis. The superficial fascia forms a fascial sheath for m. auricularis posterior. The own fascia is the extension of the tendon helmet. It extends to the neck where is involved into the formation of the sheath for m. sternocleidomastoideus, m. trapezius and venter posterior of m. digastricus. The interfascial cellular space is localized between m. trapezius and venter posterior of m. digastricus. The interfascial cellular space goes into the lateral triangle of the neck and into the sheath of m. sternocleidomastoideus. It is the major pathway for the pus spread at Bezold’s abscess. Symptoms of Bezold’s abscess are swelling and soreness in the neck.
- The periosteum is firmly spliced with the bone, especially in the attachment of m. sternocleidomastoideus, m. splenius capitis, m. longissimus capitis and venter posterior of m. digastricus.
- The subperiosteal tissue is developed weakly.
- The mastoid process of the temporal bone is located behind and below from the outer ear canal. It has conelike shape. Its lateral surfaces are rough. In the middle of the mastoid process is smooth surface which is called Shypo’s trepanation triangle. The borders of the mastoid process:
- in front − a vertical line from the top of the mastoid process through the mastoid spina suprameatum (spine of Henle) on the posterior edge of the outer ear canal;
- behind − crista mastoidea;
- from above − the horizontal line is the extension of the zygomatic arch. The cellulae mastoidea are inside the mastoid bone. The upper part of cellulae mastoidea forms the mastoid cave − antrum mastoideum. The mastoid cave communicates with the tympanic cavity through the aditus ad antrum. It opens in recessus epitympanicus. All the cells of the mastoid process open into the antrum mastoideum. Mastoid cells and antrum
mastoideum are covered by the mucous membrane. The mucous membrane is continuation of the mucosa of the tympanic cavity. Thus, the tympanic cavity and its additional cavities form a pneumatic system. This pneumatic system is filled with air through the Eustachian tube. Inflammatory exudate cannot escape through the inner opening of the auditory tube at otitis because it has adhesion oedematous mucosa. As a result, the middle ear cavity forms closed space. The purulent exudate accumulates there. It is directed through aditus ad antrium to the cave and overflows the cells of the mastoid process. It causes mastoiditis. We can remove pus from the middle ear through the posterior wall of the tympanic cavity dissecting the antrum mastoideum, which is projected at the Shypo’s triangle. The outer wall of the mastoid cave is about 1 – 2 cm. The inner wall separates it from the sulcus sigmoideus and sinus sigmoideus. The upper wall of the cave is a continuation of the mastoid tegmen tympani (roof of the tympanic cavity) and separates it from the middle cranial fossa. The lateral semicircular canal and the facial nerve are located more anteriorly from the cave. Thus, purulent exudate from the tympanic cavity may penetrate to the antrum mastoideum. It destroys the inner wall of the mastoid cave and goes into the cranial cavity or into the sigmoid sinus. It causes meningitis, sepsis, thrombophlebitis of the sigmoid sinus which are displayed clinically as McKenzie syndrome (dysphagia, aphonia, torticollis). It is caused by damage of IX, X and XI pairs of cranial nerves. The doctors make mastoidectomy in all these cases. The rupture of pus to the area of the triangle of the neck causes Bezold’s mastoiditis.
MENINGES
The cranial cavity is lined by dura mater inside which is easily separated from the bones in the fornix and firmly fixed in the skull base. Therefore, at traumas of skull epidural hematomas more prevail in the fornix (vault) of the skull. The dura mater consists of two sheets. Between them are thin layer of tissue, blood vessels and nerves. N. Burdenko used this feature of the structure for removal of defect in damaged sinus. The dura mater separates at dural reflections (also known as dural folds), places where the inner dural layer is reflected as sheet-like protrusions into the cranial cavity. There are tentorium cerebelli, falx cerebri, cerebellar falx, sellar diaphragm. The tentorium cerebelli exists between and separates the cerebellum
turcica. Both cavernous sinuses are connected through intercavernous sinuses. The cavernous sinuses and intercavernous sinuses form Ridley’s ring. It receives blood from the: - inferior ophthalmic vein(anastomoses with facial veins through profunda facial vein); - superior ophthalmic vein (anastomoses with facial veins through the angular vein) (they collect blood from the forehead); - superficial middle cerebral vein; - inferior cerebral veins; - sphenoparietal sinus and occasionally, central retinal vein, frontal tributary of the middle meningeal vein. Drainage of the cavernous sinus is via: - superior petrosal sinus to the transverse sinus; - inferior petrosal sinus directly to the jugular bulb; - venous plexus on the internal carotid artery to the pterygoid plexus; - emissary viens passing through the sphenoidal foramen, foramen ovale, foramen lacerum. The cross section of cavernous sinus has a triangular shape. The cavernous sinus transmits multiple cranial nerves to the superior orbital fissure and foramen ovale. They are: In the superior wall: - oculomotor nerve (CN III) - trochlear nerve (CN IV) In the lateral wall: - trigeminal nerve (CN V) of ophthalmic branch. Traversing the lateral sinus to the ICA: - abducents nerve (CN VI) (and a. carotis interna). The presence of these links explains the rapid spread of the infection from the soft tissues of the skull into the cavernous sinus with the development of severe diseases ─ meningitis, sepsis, brain abscess. At cavernous sinus thrombosis the Foix syndrome appears. The main symptom of cavernous sinus thrombosis is ophthalmoplegia (paralysis of the muscles of the eyeball). It is the result of paralysis of the III, IV and VI pairs of cranial nerves. The other symptomes are exophthalmia (exophthalmos), swelling of the eyelids, ptosis (drooping of the upper eyelid), immobility of the eyeball. The damage of sinus occurs with pulsating exophthalmos. Cavernous sinus is connected with the superior sagittal sinus through the Trolar’s vein. And it is connected with transverse
sinus through the Labbe’s vein. (The Trolar’s vein (v. anastomotica superior) connects v. cerebri media superficialis with sinus sagittalis superior, and v. Labbe (v. anastomotica inferior) connects v. cerebri media superficialis with sinus transversus). The doctors can make bandaging of the superior sagittal sinus in its posterior parts due to these links. The middle meningeal artery branch of the first part of the maxillary artery provides blood supply of the dura mater. It penetrates into the cranial cavity through the foramen spinosum. It lies on the inner surface of the sphenoid, parietal and temporal scales into special bone sulcus (sulci a. menigeae). The artery is divided into a frontal (anterior) and parietal (posterior) branches. The anterior branch goes upwards forming arc. It forms arc. The posterior branch goes backwards or horizontally. Artery passes in the thickness of the dura mater. It is closer to its outer sheet. Artery is accompanied by two veins. The anterior branch of artery is located in the bone canal at "pterion" (place of joint of the frontal, parietal, temporal and sphenoid bones). We must remember this when performing craniotomy. a. meningea media and its branches are often damaged. It causes the formation of epidural and subdural hematomas. The course of the anterior branch corresponds to the position of gyrus precentralis. The course of the posterior branch corresponds to the localization of temporal lobe. It is important for the diagnosis of epidural hematoma. The symptoms of an intracranial hematoma: 1. Mydriasis is the dilation of the pupil in the region of hematoma, that is anisocoria − condition characterized by an unequal size of the eye pupils. It is the result of brain injury and damage of the III pair of cranial nerves. Mydriasis is accompanied by ptosis of the upper eyelid. 2. Hemiparesis is paresis of the muscles of one half of the body on the opposite side of hematoma. It is the result of compression of the motor cortex and pyramidal tract intersection. 3. Bradycardia is strictly defined in adults as a pulse rate below 60 beats per minute. It is the result of brain stem injury, oedema, hypoxia of the brain, damage of sympathetic fibers, increase of a vagal tone. 4. The presence of "lucid intervals." The consciousness is gradually suppressed with increasing hematoma. Innervation of the dura mater is carried by r. tentorii of n. ophthalmicus, r. meningeus medius of n. maxillaris, r. meningeus (branch of n. mandibularis), which penetrates into the cranial cavity through the foramen spinosum and r. meningeus of n. vagus, that enters the cranial cavity through the foramen jugulare. Under the dura mater is the arachnoid membrane of the brain −
abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain. It causes increased intracranial pressure inside the skull and may cause progressive enlargement of the head if it occurs in childhood, at convulsions, tunnel vision, and mental disability.
SIDE AREA OF FACE
Borders:
from above − the zygomatic arch and the lower edge of the orbit;
from below − the lower edge of the lower jaw;
in front − nasobuccal fold and nasolabial fold;
behind − the rear edge of the lower jaw. Side area of face is divided into buccal and parotideomasseteric regions by line of the anterior margin of the masseter muscle. Layers: The skin is thin and mobile. It has a lot of sweat and sebaceous glands, blood and lymphatic vessels and nerve endings. The facial muscles, facial artery and veins, branch of the trigeminal and facial nerves, lymph vessels, and parotid salivary gland are localized in the subcutaneous tissue. The superficial fascia forms a fascial sheath for facial muscles and neurovascular structures of the face. Facial muscles begin from bones and are embedded into the skin. They form folds. The folds help surgeons to perform the operation. The surgeons make cuts along the folds, then the postoperative scar will be hardly noticeable. Facial muscles express our emotions. They are involved in the act of eating, breathing and speech. The facial artery and vein are located between the facial muscles. The facial artery lies at the anterior margin of masseter m. on the face. It turns round the edge of the lower jaw. It is pressed to the bone to stop bleeding at wounds of the face. The facial artery arises in the carotid triangle from the external carotid artery a little above the lingual artery and, sheltered by the ramus of the mandible, passes obliquely up beneath the digastric and stylohyoid muscles, over which it arches to enter a groove on the posterior surface of the submandibular gland. It then curves upward over the body of the mandible at the antero-inferior angle of the masseter; passes forward and upward across the cheek to the angle of the mouth, then ascends along the side of the nose, and ends at the medial commissure of the eye, under the name of the angular artery. The facial branches:
inferior labial artery;
superior labial artery;
lateral nasal branch to nasalis muscle;
angular artery − the terminal branch. The facial vein accompanies the facial artery. It begins at the medial angle of the eye as the angular vein. The facial v. begins after the confluence of supraorbitalis v. and supratrochlearis v. It anastomoses with the ophthalmic veins (vv. ophthalmica superior et inferior). The facial v. connects to retromandibular v., when it passes round the edge of the lower jaw. V. facialis communis is formed in the result of this. It empties into the internal jugular vein. The facial vein anastomoses with ophthalmic vv. and sinus cavernous, and with pterygoid plexus through deep facial vein. These anastomoses are important at the spread of inflammation on face. The retrograde blood flow is possible from facial v. into the angular v., ophthalmic inferior v. and sinus cavernosus at thrombophlebitis or furuncle or from facial v. into the deep facial vein, pterygoid plexus through v. emissaria foraminis laceri into sinus cavernous. The septic embolus penetrates into the cavernous sinus. And it causes thrombosis, meningitis, brain abscess, sepsis. The prognosis of these complications is very serious. Own fascia is a continuation of the temporal aponeurosis. It is divided into superficial and deep layers. The superficial layer forms fascial sheath for cheeks fat. The deep layer of own fascia goes into fascia buccopharyngea and continues in fascia pharyngobasillaris. Bichat fat pad is enclosed in its own capsule and is located at the front edge of the m. masseter and lateral muscle of cheek. It is turned round by ductus parotideus outside and in front of it. The cheeks fat consists of three parts, from which the temporal, orbital and pterygopalatine processes spring. Temporal process penetrates under the zygomatic arch and has a connection with subgaleal cellular space of the temporal region. Orbital process enters the infratemporal fossa. It adheres to fissura orbitalis inferior and often joins adipose body of the orbit. Pterygopalatine process has a connection with the temporal pterygoid space and penetrates through fissura pterygomaxillaris into the pterygopalatine fossa. It surrounds n. maxillaris and ganglion pterygopalatinum. Often it passes through fissura orbitalis superior in the internal base of the skull reaching the cavernous sinus. Thus the cheeks fat connects subcutaneous tissue of buccal region with temporal pterygoid space, subgaleal space of
Layers: The skin is thin and mobile. It is covered with hair. The subcutaneous tissue The branch of the ear nerve, great auricular nerve (n. auricularis magnus) and auriculotemporal nerve (n. auriculotemporalis), the buccal nerve of mandibular nerve, branch of the facial nerve, transverse facial artery (a. transversa faciei) and zygomaticofacial nerve are in the superficial fascia (fascial compartment). The own fascia (fascia parotideomasseterica) is under superficial fascia. It is attached to the zygomatic arch, and to the lower edge side of the lower jaw. It splits into two sheets and forms the capsule of the parotid gland (fascia parotidea). It penetrates into the gland between its segments. Parotid fascia moves to masseter muscle and is called masseteric fascia. In the anterior part of the parotid-masticatory area is located the masseter muscle (it begins from the zygomatic bone and the zygomatic arch and is attached to masseteric tuberosity). The muscle elevates the mandible at contraction and moves it forward. It is located in the bone and fibrous sheath. The inner surface of the muscle is adjacent to the branches of the mandible in the submasseterric space. The submasseterric space is located between the branches of the mandible and masseter muscles. There are masseteric artery, vein, nerve in the submasseteric space. The submasseteric space communicates with temporopterygoid space, interpterygoid space and Bichat fat-pad. The phlegmons can develop here. To the middle from the masseter muscle is a branch of the lower jaw. The condylar process of mandible completes temporomandibular joint. There are main components of the TMJ: caput mandibular fossa and tuberculum articulare. Dislocations of jaw occur when two bones that originally met at the joint detach. The parotid gland is located in the posterior part of the parotid-masticatory area. It is the largest salivary gland of serous type. It is surrounded by sheets of fascia parotis and muscles. It performs parotid space with arteries, veins and nerves. The borders of parotid space are:
superior – the ear canal (external auditory meatus);
inferior – the submandibular salivary gland;
anterior – rear and outer surface of masseter m., a branch of the lower jaw and medial pterygoid muscle;
posterior – sternocleidomastoid muscle, posterior belly of the digastric muscle and mastoid process;
medial – styloid process with muscles of Riolan’s bouquet (m. stylohyoideus, m. styloglossus and m. stylopharyngeus) and tissue of the anterior parapharyngeal space. In this place spatium parotideum is not closed. Pharyngeal process of gl. parotis fills the space between the styloid process and medial pterygoid muscle. It is deprived of fascial compartment (weak spot in the capsule) and is adjacent to the anterior part of the peripharyngeal space. This explains the possibility of penetration of pus from the parotid gland into the peripharyngeal cellular space, when the process is inflamed. Laterally to the parotid gland is adjacent subcutaneous fat. Fascial capsule is weakly developed. It can break at mumps (purulent parotitis). The inflammatory process spreads to the middle ear. The parotid gland is supplied with blood from parotid branches of superficial temporal artery. Venous outflow is carried out in retromandibular veih Lymph flow is carried out in nodi lymphatici parotidei superficialis et profundi. It is innervated by parotid branches of auriculotemporal n. The secretory parasympathetic preganglionic fibers come to gland from lower salivary nucleus. The secretory parasympathetic fibers consist of n. glossopharyngeus, n. tympanicus, n. petrosus minor to ganglion oticum. The postganglionic fibers are composed of n. auriculotemporalis and reach the gland. Excretory duct of parotid gl. (Stenon’s duct) begins from the front edge of the gland. It is directed forward, at a distance of 1 − 1 cm below and parallelly to the zygomatic arch on the outer surface of the masseter muscle. It lies on the top of the Bichat fat-pad and passing round front edge of the masseter muscle, turns inward. Excretory duct pierces the buccal muscle, passes under the buccal mucosa and opens in the buccal cavity between 1 and 2 upper molars. Excretory duct is projected on a line drawn from the outer ear canal to a point midway between the wing of the nose and angle of the mouth. The a. carotis externa, v. retromandibularis, n. auriculotemporalis and n. facialis are passed through the parotid gland. The external carotid artery is divided into terminal branches: a. temporalis superficialis and a. maxillaris. The retromandibular vein is a continuation of v. temporalis superficialis. It passes in front of the auricle, goes down behind the branches of the mandible laterally to the external carotid artery. It completes with facial vein behind of posterior belly of the digastric muscle. Their common trunk − v. facialis communis empties into the internal jugular vein. The auriculotemporal nerve is a branch of n. mandibularis. It begins with two roots which cover a. meningea media and are connected to one trunk. It extends along the inner surface of the
Topographic Anatomy
Course: Anatomy 1
University: Assiut University

- Discover more from:Anatomy 1Assiut University6 Documents